Abstract
Purpose
Surgical management of inflammatory bowel disease (IBD) is a challenging task. The aim of preoperative optimization (PO) is to decrease the risk of complications and reduce the length of postoperative stay. The aim of this study was to review and grade the available evidence, attain clear recommendations, and point out potential future research.
Methods
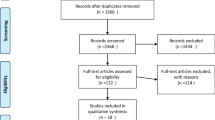
Studies were identified from electronic databases (PubMed, Embase, and Cochrane Library) and scanning reference lists in relevant papers. English-written studies examining PO in adult patients with IBD were included. Eight PO factors were investigated.
Results
Management of IBD is a multidisciplinary task. Steroid withdrawal is recommended while steroid stress dose is not recommended. Thiopurines appear to be safe, but it may be prudent to plan the procedure remotely from the last dose of an anti-TNF agent. Nutritional risk screening is recommended to unveil and correct any malnutrition. Thrombosis prophylaxis prior to surgery is well supported by evidence while extended 4-week prophylaxis needs further research. Percutaneous ultrasound or CT-guided drainage for intra-abdominal abscesses is recommended, but it is unclear for how long supplementary antibiotics (ABs) should be used. Oral AB 24 h prior to open surgery might improve outcome if given as complementary to IV perioperative AB. Mechanical bowel preparation is not supported by evidence. Comorbidities must be treated accordingly prior to surgical intervention. Smoking cessation can be beneficial for wound healing.
Conclusion
Multimodel PO intervention in IBD patients is recommended.

Similar content being viewed by others
References
Alos R, Hinojosa J (2008) Timing of surgery in Crohn’s disease: a key issue in the management. World J Gastroenterol 14(36):5532–5539
Martindale RG, Deveney CW (2013) Preoperative risk reduction: strategies to optimize outcomes. Surg Clin North Am 93(5):1041–1055. https://doi.org/10.1016/j.suc.2013.06.015
Gapasin J, Van Langenberg DR, Holtmann G, Hetzel DJ, Andrews JM (2012) Potentially avoidable surgery in inflammatory bowel disease: what proportion of patients come to resection without optimal preoperative therapy? A guidelines-based audit. Intern Med J 42(5):e84–e88. https://doi.org/10.1111/j.1445-5994.2010.02328.x
El-Hussuna A, Andersen J, Bisgaard T, Jess P, Henriksen M, Oehlenschlager J, Thorlacius-Ussing O, Olaison G (2012) Biologic treatment or immunomodulation is not associated with postoperative anastomotic complications in abdominal surgery for Crohn's disease. Scand J Gastroenterol 47(6):662–668. https://doi.org/10.3109/00365521.2012.660540
Subramanian V, Saxena S, Kang JY, Pollok RC (2008) Preoperative steroid use and risk of postoperative complications in patients with inflammatory bowel disease undergoing abdominal surgery. Am J Gastroenterol 103(9):2373–2381. https://doi.org/10.1111/j.1572-0241.2008.01942.x
El-Hussuna A, Krag A, Olaison G, Bendtsen F, Gluud LL (2013) The effect of anti-tumor necrosis factor alpha agents on postoperative anastomotic complications in Crohn's disease: a systematic review. Dis Colon Rectum 56(12):1423–1433. https://doi.org/10.1097/DCR.0b013e3182a48505
Kumar A, Auron M, Aneja A, Mohr F, Jain A, Shen B (2011) Inflammatory bowel disease: perioperative pharmacological considerations. Mayo Clin Proc 86(8):748–757. https://doi.org/10.4065/mcp.2011.0074
Jacobson S (2012) Early postoperative complications in patients with Crohn’s disease given and not given preoperative total parenteral nutrition. Scand J Gastroenterol 47(2):170–177. https://doi.org/10.3109/00365521.2011.648954
Wagner IJ, Rombeau JL (2011) Nutritional support of surgical patients with inflammatory bowel disease. Surg Clin North Am 91(4):787–803, viii. https://doi.org/10.1016/j.suc.2011.04.013
Nguyen GC (2013) IBD: postoperative VTE prophylaxis in IBD. Nature reviews. Gastroenterol Hepatol 10(1):5–6. https://doi.org/10.1038/nrgastro.2012.233
Scarpa M, Pilon F, Pengo V, Romanato G, Ruffolo C, Erroi F, Elisa B, Frego M, Ossi E, Manzato E, Angriman I (2010) Deep venous thrombosis after surgery for inflammatory bowel disease: is standard dose low molecular weight heparin prophylaxis enough? World J Surg 34(7):1629–1636. https://doi.org/10.1007/s00268-010-0490-8
Zerbib P, Koriche D, Truant S, Bouras AF, Vernier-Massouille G, Seguy D, Pruvot FR, Cortot A, Colombel JF (2010) Pre-operative management is associated with low rate of post-operative morbidity in penetrating Crohn's disease. Aliment Pharmacol Ther 32(3):459–465. https://doi.org/10.1111/j.1365-2036.2010.04369.x
Mahid SS, Minor KS, Stevens PL, Galandiuk S (2007) The role of smoking in Crohn's disease as defined by clinical variables. Dig Dis Sci 52(11):2897–2903. https://doi.org/10.1007/s10620-006-9624-0
Morar PS, Hodgkinson JD, Thalayasingam S, Koysombat K, Purcell M, Hart AL, Warusavitarne J, Faiz O (2015) Determining predictors for intra-abdominal septic complications following ileocolonic resection for Crohn’s disease-considerations in pre-operative and peri-operative optimisation techniques to improve outcome. J Crohn's Colitis 9(6):483–491. https://doi.org/10.1093/ecco-jcc/jjv051
Ananthakrishnan AN, McGinley EL (2013) Treatment of intra-abdominal abscesses in Crohn’s disease: a nationwide analysis of patterns and outcomes of care. Dig Dis Sci 58(7):2013–2018. https://doi.org/10.1007/s10620-013-2579-z
Muller-Wille R, Iesalnieks I, Dornia C, Ott C, Jung EM, Friedrich C, Schill G, Hoffstetter P, Zorger N, Schreyer AG (2011) Influence of percutaneous abscess drainage on severe postoperative septic complications in patients with Crohn's disease. Int J Color Dis 26(6):769–774. https://doi.org/10.1007/s00384-011-1135-6
Xie Y, Zhu W, Li N, Li J (2012) The outcome of initial percutaneous drainage versus surgical drainage for intra-abdominal abscesses in Crohn’s disease. Int J Color Dis 27(2):199–206. https://doi.org/10.1007/s00384-011-1338-x
Efron JE, Young-Fadok TM (2007) Preoperative optimization of Crohn's disease. Clin Colon Rectal Surg 20(4):303–308. https://doi.org/10.1055/s-2007-991029
Sharma A, Chinn BT (2013) Preoperative optimization of Crohn disease. Clin Colon Rectal Surg 26(2):75–79. https://doi.org/10.1055/s-0033-1348044
Spinelli A, Allocca M, Jovani M, Danese S (2014) Review article: optimal preparation for surgery in Crohn’s disease. Aliment Pharmacol Ther 40(9):1009–1022. https://doi.org/10.1111/apt.12947
Braga M, Ljungqvist O, Soeters P, Fearon K, Weimann A, Bozzetti F (2009) ESPEN guidelines on parenteral nutrition: surgery. Clin Nutr (Edinburgh, Scotland) 28(4):378–386. https://doi.org/10.1016/j.clnu.2009.04.002
Weimann A, Braga M, Harsanyi L, Laviano A, Ljungqvist O, Soeters P, Jauch KW, Kemen M, Hiesmayr JM, Horbach T, Kuse ER, Vestweber KH (2006) ESPEN guidelines on enteral nutrition: surgery including organ transplantation. Clin Nutr (Edinburgh, Scotland) 25(2):224–244. https://doi.org/10.1016/j.clnu.2006.01.015
Zangenberg MS, El-Hussuna A (2015) Preoperative optimization of patients with inflammatory bowel disease undergoing gastrointestinal surgery: PRISMA protocol. Slagelse Hospital
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schunemann HJ (2011) GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64(4):383–394. https://doi.org/10.1016/j.jclinepi.2010.04.026
Ahmed Ali U, Martin ST, Rao AD, Kiran RP (2014) Impact of preoperative immunosuppressive agents on postoperative outcomes in Crohn's disease. Dis Colon Rectum 57(5):663–674. https://doi.org/10.1097/dcr.0000000000000099
El-Hussuna A, Theede K, Olaison G (2014) Increased risk of post-operative complications in patients with Crohn's disease treated with anti-tumour necrosis factor alpha agents - a systematic review. Dan Med J 61(12):A4975
Ferrante M, D'Hoore A, Vermeire S, Declerck S, Noman M, Van Assche G, Hoffman I, Rutgeerts P, Penninckx F (2009) Corticosteroids but not infliximab increase short-term postoperative infectious complications in patients with ulcerative colitis. Inflamm Bowel Dis 15(7):1062–1070. https://doi.org/10.1002/ibd.20863
Lau C, Dubinsky M, Melmed G, Vasiliauskas E, Berel D, McGovern D, Ippoliti A, Shih D, Targan S, Fleshner P (2015) The impact of preoperative serum anti-TNFalpha therapy levels on early postoperative outcomes in inflammatory bowel disease surgery. Ann Surg 261(3):487–496. https://doi.org/10.1097/sla.0000000000000757
Myrelid P, Olaison G, Sjodahl R, Nystrom PO, Almer S, Andersson P (2009) Thiopurine therapy is associated with postoperative intra-abdominal septic complications in abdominal surgery for Crohn’s disease. Dis Colon Rectum 52(8):1387–1394. https://doi.org/10.1007/DCR.0b013e3181a7ba96
Nelson RL, Gladman E, Barbateskovic M (2014) Antimicrobial prophylaxis for colorectal surgery. Cochrane Database Syst Rev (5):CD001181. https://doi.org/10.1002/14651858.CD001181.pub4
Selvaggi F, Pellino G, Canonico S, Sciaudone G (2015) Effect of preoperative biologic drugs on complications and function after restorative proctocolectomy with primary ileal pouch formation: systematic review and meta-analysis. Inflamm Bowel Dis 21(1):79–92. https://doi.org/10.1097/mib.0000000000000232
Subramanian V, Pollok RC, Kang JY, Kumar D (2006) Systematic review of postoperative complications in patients with inflammatory bowel disease treated with immunomodulators. Br J Surg 93(7):793–799. https://doi.org/10.1002/bjs.5375
Syed A, Cross RK, Flasar MH (2013) Anti-tumor necrosis factor therapy is associated with infections after abdominal surgery in Crohn’s disease patients. Am J Gastroenterol 108(4):583–593. https://doi.org/10.1038/ajg.2012.464
Waterman M, Xu W, Dinani A, Steinhart AH, Croitoru K, Nguyen GC, McLeod RS, Greenberg GR, Cohen Z, Silverberg MS (2013) Preoperative biological therapy and short-term outcomes of abdominal surgery in patients with inflammatory bowel disease. Gut 62(3):387–394. https://doi.org/10.1136/gutjnl-2011-301495
Yang Z, Wu Q, Wu K, Fan D (2010) Meta-analysis: pre-operative infliximab treatment and short-term post-operative complications in patients with ulcerative colitis. Aliment Pharmacol Ther 31(4):486–492. https://doi.org/10.1111/j.1365-2036.2009.04204.x
Yang ZP, Hong L, Wu Q, Wu KC, Fan DM (2014) Preoperative infliximab use and postoperative complications in Crohn’s disease: a systematic review and meta-analysis. Int J Surg (London, England) 12(3):224–230. https://doi.org/10.1016/j.ijsu.2013.12.015
Bemelman WA, Warusavitarne J, Sampietro GM, Serclova Z, Zmora O, Luglio G, de Buck van Overstraeten A, Burke JP, Buskens CJ, Francesco C, Amil Dias J, Eliakim R, Elosua T, Gecim IE, Kolacek S, Kierkus J, Kolho KL, Lefevre JH, Millan M, Panis Y, Pinkney T, Russell RK, Shwaartz C, Vaizey C, Yassin N, D'Hoore A, European Cs, Colitis O, European Society of C (2017) ECCO-ESCP consensus on surgery for Crohn’s disease. J Crohn's Colitis. https://doi.org/10.1093/ecco-jcc/jjx061
Wakim JH, Sledge KC (2006) Anesthetic implications for patients receiving exogenous corticosteroids. AANA J 74(2):133–139
de Lange DW, Kars M (2008) Perioperative glucocorticosteroid supplementation is not supported by evidence. Eur J Intern Med 19(6):461–467. https://doi.org/10.1016/j.ejim.2007.12.004
Kelly KN, Domajnko B (2013) Perioperative stress-dose steroids. Clin Colon Rectal Surg 26(3):163–167. https://doi.org/10.1055/s-0033-1351132
Marik PE, Varon J (2008) Requirement of perioperative stress doses of corticosteroids: a systematic review of the literature. Arch Surg (Chicago, Ill : 1960) 143(12):1222–1226. https://doi.org/10.1001/archsurg.143.12.1222
Brown CJ, Buie WD (2001) Perioperative stress dose steroids: do they make a difference? J Am Coll Surg 193(6):678–686
Yong SL, Coulthard P, Wrzosek A (2012) Supplemental perioperative steroids for surgical patients with adrenal insufficiency. Cochrane Database Syst Rev 12:Cd005367. https://doi.org/10.1002/14651858.CD005367.pub3
Zaghiyan K, Melmed GY, Berel D, Ovsepyan G, Murrell Z, Fleshner P (2014) A prospective, randomized, noninferiority trial of steroid dosing after major colorectal surgery. Ann Surg 259(1):32–37. https://doi.org/10.1097/SLA.0b013e318297adca
Borrelli O, Cordischi L, Cirulli M, Paganelli M, Labalestra V, Uccini S, Russo PM, Cucchiara S (2006) Polymeric diet alone versus corticosteroids in the treatment of active pediatric Crohn’s disease: a randomized controlled open-label trial. Clin Gastroenterol Hepatol: Off Clin Pract J Am Gastroenterol Assoc 4(6):744–753. https://doi.org/10.1016/j.cgh.2006.03.010
Yamamoto T, Nakahigashi M, Saniabadi AR, Iwata T, Maruyama Y, Umegae S, Matsumoto K (2007) Impacts of long-term enteral nutrition on clinical and endoscopic disease activities and mucosal cytokines during remission in patients with Crohn’s disease: a prospective study. Inflamm Bowel Dis 13(12):1493–1501. https://doi.org/10.1002/ibd.20238
Alves A, Panis Y, Bouhnik Y, Pocard M, Vicaut E, Valleur P (2007) Risk factors for intra-abdominal septic complications after a first ileocecal resection for Crohn’s disease: a multivariate analysis in 161 consecutive patients. Dis Colon Rectum 50(3):331–336. https://doi.org/10.1007/s10350-006-0782-0
Salinas H, Dursun A, Konstantinidis I, Nguyen D, Shellito P, Hodin R, Bordeianou L (2012) Does preoperative total parenteral nutrition in patients with ulcerative colitis produce better outcomes? Int J Color Dis 27(11):1479–1483. https://doi.org/10.1007/s00384-012-1535-2
Yao GX, Wang XR, Jiang ZM, Zhang SY, Ni AP (2005) Role of perioperative parenteral nutrition in severely malnourished patients with Crohn's disease. World J Gastroenterol 11(36):5732–5734
Li G, Ren J, Wang G, Hu D, Gu G, Liu S, Ren H, Wu X, Li J (2014) Preoperative exclusive enteral nutrition reduces the postoperative septic complications of fistulizing Crohn’s disease. Eur J Clin Nutr 68(4):441–446. https://doi.org/10.1038/ejcn.2014.16
Li Y, Zuo L, Zhu W, Gong J, Zhang W, Gu L, Guo Z, Cao L, Li N, Li J (2015) Role of exclusive enteral nutrition in the preoperative optimization of patients with Crohn's disease following immunosuppressive therapy. Medicine 94(5):e478. https://doi.org/10.1097/md.0000000000000478
Kondrup J, Allison SP, Elia M, Vellas B, Plauth M (2003) ESPEN guidelines for nutrition screening 2002. Clin Nutr (Edinburgh, Scotland) 22(4):415–421
Murthy SK, Nguyen GC (2011) Venous thromboembolism in inflammatory bowel disease: an epidemiological review. Am J Gastroenterol 106(4):713–718. https://doi.org/10.1038/ajg.2011.53
Twig G, Zandman-Goddard G, Szyper-Kravitz M, Shoenfeld Y (2005) Systemic thromboembolism in inflammatory bowel disease: mechanisms and clinical applications. Ann N Y Acad Sci 1051:166–173. https://doi.org/10.1196/annals.1361.058
Yuhara H, Steinmaus C, Corley D, Koike J, Igarashi M, Suzuki T, Mine T (2013) Meta-analysis: the risk of venous thromboembolism in patients with inflammatory bowel disease. Aliment Pharmacol Ther 37(10):953–962. https://doi.org/10.1111/apt.12294
Papa A, Papa V, Marzo M, Scaldaferri F, Sofo L, Rapaccini GL, Danese S, Gasbarrini A (2015) Prevention and treatment of venous thromboembolism in patients with IBD: a trail still climbing. Inflamm Bowel Dis 21(5):1204–1213. https://doi.org/10.1097/mib.0000000000000310
Gross ME, Vogler SA, Mone MC, Sheng X, Sklow B (2014) The importance of extended postoperative venous thromboembolism prophylaxis in IBD: a National Surgical Quality Improvement Program analysis. Dis Colon Rectum 57(4):482–489. https://doi.org/10.1097/dcr.0000000000000090
Kaplan GG, Lim A, Seow CH, Moran GW, Ghosh S, Leung Y, Debruyn J, Nguyen GC, Hubbard J, Panaccione R (2015) Colectomy is a risk factor for venous thromboembolism in ulcerative colitis. World J Gastroenterol 21(4):1251–1260. https://doi.org/10.3748/wjg.v21.i4.1251
Merrill A, Millham F (2012) Increased risk of postoperative deep vein thrombosis and pulmonary embolism in patients with inflammatory bowel disease: a study of National Surgical Quality Improvement Program patients. Arch Surg (Chicago, Ill : 1960) 147(2):120–124. https://doi.org/10.1001/archsurg.2011.297
O'Connor OJ, Cahill RA, Kirwan WO, Redmond HP (2005) The incidence of postoperative venous thrombosis among patients with ulcerative colitis. Ir J Med Sci 174(3):20–22
Wallaert JB, De Martino RR, Marsicovetere PS, Goodney PP, Finlayson SR, Murray JJ, Holubar SD (2012) Venous thromboembolism after surgery for inflammatory bowel disease: are there modifiable risk factors? Data from ACS NSQIP. Dis Colon Rectum 55(11):1138–1144. https://doi.org/10.1097/DCR.0b013e3182698f60
Vedovati MC, Becattini C, Rondelli F, Boncompagni M, Camporese G, Balzarotti R, Mariani E, Flamini O, Pucciarelli S, Donini A, Agnelli G (2014) A randomized study on 1-week versus 4-week prophylaxis for venous thromboembolism after laparoscopic surgery for colorectal cancer. Ann Surg 259(4):665–669. https://doi.org/10.1097/sla.0000000000000340
Bafford AC, Coakley B, Powers S, Greenwald D, Ha CY, Weintraub J, Chessin DB, Gorfine SR, Bauer JJ (2012) The clinical impact of preoperative percutaneous drainage of abdominopelvic abscesses in patients with Crohn’s disease. Int J Color Dis 27(7):953–958. https://doi.org/10.1007/s00384-011-1401-7
Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, Fish DN, Napolitano LM, Sawyer RG, Slain D, Steinberg JP, Weinstein RA (2013) Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect 14(1):73–156. https://doi.org/10.1089/sur.2013.9999
Oshima T, Takesue Y, Ikeuchi H, Matsuoka H, Nakajima K, Uchino M, Tomita N, Sasako M (2013) Preoperative oral antibiotics and intravenous antimicrobial prophylaxis reduce the incidence of surgical site infections in patients with ulcerative colitis undergoing IPAA. Dis Colon Rectum 56(10):1149–1155. https://doi.org/10.1097/DCR.0b013e31829f71a0
Remzi FH, Lavryk OA, Ashburn JH, Hull TL, Lavery IC, Dietz DW, Kessler H, Church JM (2017) Restorative proctocolectomy: an example of how surgery evolves in response to paradigm shifts in care. Colorectal Dis: Off J Assoc Coloproctol G B Irel. https://doi.org/10.1111/codi.13699
Morris MS, Graham LA, Chu DI, Cannon JA, Hawn MT (2015) Oral antibiotic bowel preparation significantly reduces surgical site infection rates and readmission rates in elective colorectal surgery. Ann Surg 261(6):1034–1040. https://doi.org/10.1097/sla.0000000000001125
Spinelli A, Bazzi P, Sacchi M, Danese S, Fiorino G, Malesci A, Gentilini L, Poggioli G, Montorsi M (2013) Short-term outcomes of laparoscopy combined with enhanced recovery pathway after ileocecal resection for Crohn's disease: a case-matched analysis. J Gastrointest Surg: Off J Soc Surg Aliment Tract 17(1):126–132; discussion p.132. https://doi.org/10.1007/s11605-012-2012-5
Cao F, Li J, Li F (2012) Mechanical bowel preparation for elective colorectal surgery: updated systematic review and meta-analysis. Int J Color Dis 27(6):803–810. https://doi.org/10.1007/s00384-011-1361-y
Güenage KF, Matos D, Wille-Jørgensen P (2011) Mechanical bowel preparation for elective colorectal surgery. Cochrane Database Syst Rev (9):CD001544. https://doi.org/10.1002/14651858.CD001544.pub4
Zhu QD, Zhang QY, Zeng QQ, Yu ZP, Tao CL, Yang WJ (2010) Efficacy of mechanical bowel preparation with polyethylene glycol in prevention of postoperative complications in elective colorectal surgery: a meta-analysis. Int J Color Dis 25(2):267–275. https://doi.org/10.1007/s00384-009-0834-8
Shwaartz C, Fields AC, Sobrero M, Divino CM (2017) Does bowel preparation for inflammatory bowel disease surgery matter? Colorectal Dis: Off J Assoc Coloproctol G B Irel. https://doi.org/10.1111/codi.13693
Juneja M, Baidoo L, Schwartz MB, Barrie A 3rd, Regueiro M, Dunn M, Binion DG (2012) Geriatric inflammatory bowel disease: phenotypic presentation, treatment patterns, nutritional status, outcomes, and comorbidity. Dig Dis Sci 57(9):2408–2415. https://doi.org/10.1007/s10620-012-2083-x
Pinto RA, Canedo J, Murad-Regadas S, Regadas SF, Weiss EG, Wexner SD (2011) Ileal pouch-anal anastomosis in elderly patients: is there a difference in morbidity compared with younger patients? Colorectal Dis: Off J Assoc Coloproctol G B Irel 13(2):177–183. https://doi.org/10.1111/j.1463-1318.2009.02097.x
Kaplan GG, Hubbard J, Panaccione R, Shaheen AA, Quan H, Nguyen GC, Dixon E, Ghosh S, Myers RP (2011) Risk of comorbidities on postoperative outcomes in patients with inflammatory bowel disease. Arch Surg (Chicago, Ill : 1960) 146(8):959–964. https://doi.org/10.1001/archsurg.2011.194
Picco MF, Bayless TM (2003) Tobacco consumption and disease duration are associated with fistulizing and stricturing behaviors in the first 8 years of Crohn's disease. Am J Gastroenterol 98(2):363–368. https://doi.org/10.1111/j.1572-0241.2003.07240.x
Pittet V, Rogler G, Michetti P, Fournier N, Vader JP, Schoepfer A, Mottet C, Burnand B, Froehlich F (2013) Penetrating or stricturing diseases are the major determinants of time to first and repeat resection surgery in Crohn's disease. Digestion 87(3):212–221. https://doi.org/10.1159/000350954
Timmer A, Sutherland LR, Martin F (1998) Oral contraceptive use and smoking are risk factors for relapse in Crohn’s disease. The Canadian Mesalamine for Remission of Crohn's Disease Study Group. Gastroenterology 114(6):1143–1150
Cosnes J, Beaugerie L, Carbonnel F, Gendre JP (2001) Smoking cessation and the course of Crohn’s disease: an intervention study. Gastroenterology 120(5):1093–1099. https://doi.org/10.1053/gast.2001.23231
Beaugerie L, Massot N, Carbonnel F, Cattan S, Gendre JP, Cosnes J (2001) Impact of cessation of smoking on the course of ulcerative colitis. Am J Gastroenterol 96(7):2113–2116. https://doi.org/10.1111/j.1572-0241.2001.03944.x
Joyce MR, Hannaway CD, Strong SA, Fazio VW, Kiran RP (2013) Impact of smoking on disease phenotype and postoperative outcomes for Crohn's disease patients undergoing surgery. Langenbeck's Arch Surg 398(1):39–45. https://doi.org/10.1007/s00423-011-0865-9
Reese GE, Nanidis T, Borysiewicz C, Yamamoto T, Orchard T, Tekkis PP (2008) The effect of smoking after surgery for Crohn’s disease: a meta-analysis of observational studies. Int J Color Dis 23(12):1213–1221. https://doi.org/10.1007/s00384-008-0542-9
Sharma A, Deeb AP, Iannuzzi JC, Rickles AS, Monson JR, Fleming FJ (2013) Tobacco smoking and postoperative outcomes after colorectal surgery. Ann Surg 258(2):296–300. https://doi.org/10.1097/SLA.0b013e3182708cc5
de Groof EJ, Carbonnel F, Buskens CJ, Bemelman WA (2014) Abdominal abscess in Crohn’s disease: multidisciplinary management. Dig Dis (Basel, Switzerland) 32(Suppl 1):103–109. https://doi.org/10.1159/000367859
Gasparetto M, Angriman I, Guariso G (2015) The multidisciplinary health care team in the management of stenosis in Crohn’s disease. J Multidiscip Healthc 8:167–179. https://doi.org/10.2147/jmdh.s38729
Habal FM, Huang VW (2012) Review article: a decision-making algorithm for the management of pregnancy in the inflammatory bowel disease patient. Aliment Pharmacol Ther 35(5):501–515. https://doi.org/10.1111/j.1365-2036.2011.04967.x
Hernandez-Sampelayo P, Seoane M, Oltra L, Marin L, Torrejon A, Vera MI, Garcia V, Lazaro P, Parody E, Blasco AJ, Casellas F (2010) Contribution of nurses to the quality of care in management of inflammatory bowel disease: a synthesis of the evidence. J Crohn's Colitis 4(6):611–622. https://doi.org/10.1016/j.crohns.2010.08.009
Louis E, Dotan I, Ghosh S, Mlynarsky L, Reenaers C, Schreiber S (2015) Optimising the inflammatory bowel disease unit to improve quality of care: expert recommendations. J Crohn's Colitis 9(8):685–691. https://doi.org/10.1093/ecco-jcc/jjv085
Ricci C, Lanzarotto F, Lanzini A (2008) The multidisciplinary team for management of inflammatory bowel diseases. Dig Liver Dis: Off J Italian Soc Gastroenterol Italian Assoc Study Liver 40(Suppl 2):S285–S288. https://doi.org/10.1016/s1590-8658(08)60539-3
Filipovic BR, Filipovic BF (2014) Psychiatric comorbidity in the treatment of patients with inflammatory bowel disease. World J Gastroenterol 20(13):3552–3563. https://doi.org/10.3748/wjg.v20.i13.3552
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62(10):e1–34. https://doi.org/10.1016/j.jclinepi.2009.06.006
Author information
Authors and Affiliations
Corresponding author
Appendix. Search strategy from PubMed
Appendix. Search strategy from PubMed
((((((((((((nutritional support) OR ((enteral nutrition) OR parenteral nutrition))) OR ((((((((((((((((((((optimal preparation) OR optimisation) OR optimise) OR optimize) OR optimization) OR optimal preparation) OR preparation)) OR thrombosis prophylaxis) OR ((nutritional support) OR nutritional support[MeSH Major Topic])) OR nutritional support[MeSH Major Topic]) OR preoperative sepsis treatment) OR bowel rest) OR anticoagulants) OR nutritional support) OR period, preoperative) OR care, preoperative) OR ((sepsis therapy) OR sepsis treatment)) OR sepsis treatment) OR sepsis therapy))) AND ((surgery) OR colorectal surgery)) AND (Inflammatory bowel disease OR ibd OR Crohn disease OR crohn’s disease OR Colitis ulcerative)))) OR (((((“inflammatory bowel diseases”[MeSH Terms] OR (“inflammatory”[All Fields] AND “bowel”[All Fields] AND “diseases”[All Fields]) OR “inflammatory bowel diseases”[All Fields] OR (“inflammatory”[All Fields] AND “bowel”[All Fields] AND “disease”[All Fields]) OR “inflammatory bowel disease”[All Fields]) OR ibd[All Fields] OR (“crohn disease”[MeSH Terms] OR (“crohn”[All Fields] AND “disease”[All Fields]) OR “crohn disease”[All Fields]) OR (“crohn disease”[MeSH Terms] OR (“crohn”[All Fields] AND “disease”[All Fields]) OR “crohn disease”[All Fields] OR (“crohn’s”[All Fields] AND “disease”[All Fields]) OR “crohn’s disease”[All Fields]) OR (“colitis, ulcerative”[MeSH Terms] OR (“colitis”[All Fields] AND “ulcerative”[All Fields]) OR “ulcerative colitis”[All Fields] OR (“colitis”[All Fields] AND “ulcerative”[All Fields]) OR “colitis ulcerative”[All Fields]))) AND ((((“surgery”[Subheading] OR “surgery”[All Fields] OR “surgical procedures, operative”[MeSH Terms] OR (“surgical”[All Fields] AND “procedures”[All Fields] AND “operative”[All Fields]) OR “operative surgical procedures”[All Fields] OR “surgery”[All Fields] OR “general surgery”[MeSH Terms] OR (“general”[All Fields] AND “surgery”[All Fields]) OR “general surgery”[All Fields]) OR (“colorectal surgery”[MeSH Terms] OR (“colorectal”[All Fields] AND “surgery”[All Fields]) OR “colorectal surgery”[All Fields])) OR (“postoperative complications”[MeSH Terms] OR (“postoperative”[All Fields] AND “complications”[All Fields]) OR “postoperative complications”[All Fields])) OR ((“postoperative period”[MeSH Terms] OR (“postoperative”[All Fields] AND “period”[All Fields]) OR “postoperative period”[All Fields] OR “postoperative”[All Fields]) AND (“infection”[MeSH Terms] OR “infection”[All Fields] OR “infections”[All Fields])))) AND ((((((((“biological products”[MeSH Terms] OR (“biological”[All Fields] AND “products”[All Fields]) OR “biological products”[All Fields] OR “biologics”[All Fields]) OR “biological agent”[All Fields]) OR “biological agents”[All Fields]) OR (“biosimilar pharmaceuticals”[MeSH Terms] OR (“biosimilar”[All Fields] AND “pharmaceuticals”[All Fields]) OR “biosimilar pharmaceuticals”[All Fields])) OR (((“infliximab”[MeSH Terms] OR “infliximab”[All Fields] OR “remicade”[All Fields]) OR (“adalimumab”[MeSH Terms] OR “adalimumab”[All Fields] OR “humira”[All Fields])) OR (((((((“antibodies, monoclonal”[MeSH Terms] OR (“antibodies”[All Fields] AND “monoclonal”[All Fields]) OR “monoclonal antibodies”[All Fields] OR (“antibodies”[All Fields] AND “monoclonal”[All Fields]) OR “antibodies, monoclonal”[All Fields]) OR (“PEG-modified tumor necrosis factor-alpha”[Supplementary Concept] OR “PEG-modified tumor necrosis factor- alpha”[All Fields] OR "peg modified tumor necrosis factor alpha"[All Fields])) OR “tumor necrosis factor-alpha/antagonists and inhibitors”[Mesh Terms]) OR (anti[All Fields] AND tnf[All Fields])) OR anti-tnf[All Fields]) OR (“adalimumab”[MeSH Terms] OR “adalimumab”[All Fields])) OR (“infliximab”[MeSH Terms] OR “infliximab”[All Fields])))) OR ((((“steroids”[MeSH Terms] OR “steroids”[All Fields]) OR ((“Stress”[Journal] OR “stress”[All Fields]) AND dose[All Fields])) OR (“glucocorticoids”[Pharmacological Action] OR “glucocorticoids”[MeSH Terms] OR “glucocorticoids”[All Fields])) AND scheme[All Fields])) OR ((“comorbidity”[MeSH Terms] OR “comorbidity”[All Fields]) OR (“comorbidity”[MeSH Terms] OR “comorbidity”[All Fields] OR “comorbidities”[All Fields]))) OR (((“interdisciplinary studies”[MeSH Terms] OR (“interdisciplinary”[All Fields] AND “studies”[All Fields]) OR “interdisciplinary studies”[All Fields] OR “multidisciplinary”[All Fields]) OR ((“interdisciplinary studies”[MeSH Terms] OR (“interdisciplinary”[All Fields] AND “studies”[All Fields]) OR “interdisciplinary studies”[All Fields] OR “multidisciplinary”[All Fields]) AND teamwork[All Fields])) OR ((“interdisciplinary studies”[MeSH Terms] OR (“interdisciplinary”[All Fields] AND “studies”[All Fields]) OR “interdisciplinary studies”[All Fields] OR “multidisciplinary”[All Fields]) AND team[All Fields]))))) OR (((((((“Antibiotic Prophylaxis”[Mesh]) OR “Anti-Bacterial Agents”[Mesh])) OR (antibiotics OR “preoperative antibiotics” OR “anti bacterial prophylaxis”))) AND (((((“preoperative period” OR optimization OR preparation OR “optimal preparation” OR presurgery)) AND (“inflammatory bowel disease” OR IBD OR crohn’s))) OR ((((“Preoperative Period”[Mesh]) OR “Preoperative Care”[Mesh])) AND “Inflammatory Bowel Diseases”[Mesh]))))) OR ((((((((“psychological prehabilitation” OR “psychological interventon” OR “preoperative psychology”)) OR (“mental support” OR “mental health” OR psycotherapy OR “psychological support”))) AND (((((“preoperative period” OR optimization OR preparation OR “optimal preparation” OR presurgery)) AND (“inflammatory bowel disease” OR IBD OR crohn’s))) OR ((((“Preoperative Period”[Mesh]) OR “Preoperative Care”[Mesh])) AND “Inflammatory Bowel Diseases”[Mesh])))) OR (((((((“preoperative period” OR optimization OR preparation OR “optimal preparation” OR presurgery)) AND (“inflammatory bowel disease” OR IBD OR crohn’s))) OR ((((“Preoperative Period”[Mesh]) OR “Preoperative Care”[Mesh])) AND “Inflammatory Bowel Diseases”[Mesh]))) AND (“Smoking Cessation”[Mesh] OR smoking OR cigarette))))) OR ((((((((“preoperative period” OR optimization OR preparation OR “optimal preparation” OR presurgery)) AND (“inflammatory bowel disease” OR IBD OR crohn’s))) OR ((((“Preoperative Period”[Mesh]) OR “Preoperative Care”[Mesh])) AND “Inflammatory Bowel Diseases”[Mesh]))) AND (“bowel preparation” OR “mechanical bowel preparation” OR “colonic preparation” OR “colonic clensing”))) Filters: Publication date from 2005/01/01 to 2015/07/31; Humans.
Results ➔ 2349 items.
Similar searches were conducted in EMbase and Cochrane Library. Exact search strategies for those databases can be requested if necessary.
Rights and permissions
About this article
Cite this article
Zangenberg, M.S., Horesh, N., Kopylov, U. et al. Preoperative optimization of patients with inflammatory bowel disease undergoing gastrointestinal surgery: a systematic review. Int J Colorectal Dis 32, 1663–1676 (2017). https://doi.org/10.1007/s00384-017-2915-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-017-2915-4