Abstract
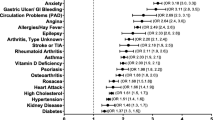
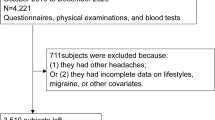
Regular lifestyle behaviors (RLBs) of sleep, exercise, mealtime pattern and hydration status independently affect migraine occurrence. We aimed herein to evaluate the differences in migraine occurrence among participants who do and do not maintain the RLB triumvirate. Cases of chronic migraine (CM) and referents of episodic migraine (EM) ≥aged 15 years with charts regularly documenting RLB notes were continuously enrolled from a retrospective case–referent cohort study performed on electronic chart review from January 1, 2014 to January 1, 2015 at the Stanford Headache and Facial Pain Program. Association between RLB prevalence and migraine occurrence was studied. 175 CM and 175 EM patients were enrolled (mean age 44.4 years, 22 % males). Migraine was diagnosed according to the ICHD-3 beta criteria, and was confirmed by a Headache Specialist attending the Clinic. The CM cohort (22 %) exhibited less RLB than the EM cohort (69 %), with crude odds ratio of 0.13 (95 % confidence interval or CI 0.08–0.21). The adjusted odds ratio and adjusted relative risk between RLB+, Meds+ (those taking medication) and CM were 0.67 (95 % CI 0.32–1.40) and 0.74 (95 % CI 0.43–1.28), indicating no significant effect modification. Engaging in regular lifestyle behavior helps quell chronic migraine.




Similar content being viewed by others
References
Buse DC, Andrasik F (2009) Behavioral medicine for migraine. Neurol Clin 27(2):445–465
Sarabdjitsingh RA et al (2010) Recovery from disrupted ultradian glucocorticoid rhythmicity reveals a dissociation between hormonal and behavioural stress responsiveness. J Neuroendocrinol 22(8):862–871
Munch M, Bromundt V (2012) Light and chronobiology: implications for health and disease. Dialogues Clin Neurosci 14(4):448–453
Hashimoto S, Honma S, Honma K (2007) Sleep and biological rhythms. Nihon Yakurigaku Zasshi 129(6):400–403
Kelman L, Rains JC (2005) Headache and sleep: examination of sleep patterns and complaints in a large clinical sample of migraineurs. Headache 45(7):904–910
Hindiyeh NA, Krusz JC, Cowan RP (2013) Does exercise make migraines worse and tension type headaches better? Curr Pain Headache Rep 17(12):380
Darabaneanu S et al (2011) Aerobic exercise as a therapy option for migraine: a pilot study. Int J Sports Med 32(6):455–460
Gil-Martinez A et al (2013) Therapeutic exercise as treatment for migraine and tension-type headaches: a systematic review of randomised clinical trials. Rev Neurol 57(10):433–443
Molarius A, Tegelberg A, Ohrvik J (2008) Socio-economic factors, lifestyle, and headache disorders—a population-based study in Sweden. Headache 48(10):1426–1437
Spigt M et al (2012) A randomized trial on the effects of regular water intake in patients with recurrent headaches. Fam Pract 29(4):370–375
Varkey E et al (2011) Exercise as migraine prophylaxis: a randomized study using relaxation and topiramate as controls. Cephalalgia 31(14):1428–1438
Martin PR, MacLeod C (2009) Behavioral management of headache triggers: avoidance of triggers is an inadequate strategy. Clin Psychol Rev 29(6):483–495
Wells RE et al (2014) Meditation for migraines: a pilot randomized controlled trial. Headache 54(9):1484–1495
Houle TT et al (2012) Stress and sleep duration predict headache severity in chronic headache sufferers. Pain 153(12):2432–2440
Hufnagl KN, Peroutka SJ (2002) Glucose regulation in headache: implications for dietary management. Expert Rev Neurother 2(3):311–317
Graham JR (1952) The natural history of migraine: some observations and a hypothesis. Trans Am Clin Climatol Assoc 64:61–73 (discussion 73–74)
Andrasik F, Buse DC, Grazzi L (2009) Behavioral medicine for migraine and medication overuse headache. Curr Pain Headache Rep 13(3):241–248
Calhoun AH, Ford S (2007) Behavioral sleep modification may revert transformed migraine to episodic migraine. Headache 47(8):1178–1183
Lowe HJ et al (2009) STRIDE—an integrated standards-based translational research informatics platform. AMIA Annu Symp Proc 2009:391–395
Dupont WD (1988) Power calculations for matched case–control studies. Biometrics 44(4):1157–1168
Headache Classification Committee of the International Headache (2013) The international classification of headache disorders, 3rd edition (beta version). Cephalalgia 33(9):629–808
von Elm E et al (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ 85(11):867–872
D’Agostino RB (1986) Tests for normal distribution. In: D’Agostino RB, Stephens MA (eds) Goodness-of-fit techniques. Marcel Dekker, New York
Welch BL (1947) The generalisation of student’s problems when several different population variances are involved. Biometrika 34(1–2):28–35
Woldeamanuel YW, Cowan RP (2016) Global migraine epidemiology: systematic review and meta-analysis of 302 community-based studies involving 6,216,995 participants. Headache
Armitage CJ, Norman P, Conner M (2002) Can the theory of planned behaviour mediate the effects of age, gender and multidimensional health locus of control? Br J Health Psychol 7:299–316
Norman P et al (1998) Health locus of control and health behaviour. J Health Psychol 3(2):171–180
Acknowledgments
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Woldeamanuel, Y.W., Cowan, R.P. The impact of regular lifestyle behavior in migraine: a prevalence case–referent study. J Neurol 263, 669–676 (2016). https://doi.org/10.1007/s00415-016-8031-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-016-8031-5