Abstract
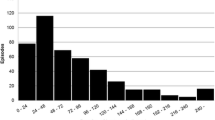
Healthcare-associated Staphylococcus aureus bacteremia (HA-SAB) is an increasingly frequently observed complication of medical treatment. Current guidelines recommend evaluation with echocardiography and preferably transesophageal echocardiography for the exclusion of infectious endocarditis (IE). We performed a retrospective analysis of all patients with HA-SAB between 1 January 2007 and 31 July 2012. Patients were divided into those with a high degree of clinical suspicion of IE (prosthetic intracardiac device, hemodialysis or positive blood cultures for 4 days or more) or those with a low degree of clinical suspicion of IE (absence of high-risk features based on previous literature as strong indicators of endocarditis). Three hundred and fifty-eight patients with HA-SAB were evaluated to determine the prevalence of IE, including 298 (83 %) who had echocardiography. Fourteen patients (4 %) had a final diagnosis of IE after echocardiography. In the group with a high degree of clinical suspicion 11 out of 84 patients (13 %) had IE. In the group with a low degree of clinical suspicion group 3 out 274 patients (1.1 %) had IE. HA-SAB has a low rate of IE, especially in the absence of high-risk features such as prolonged bacteremia, intracardiac prosthetic devices, and hemodialysis. Echocardiographic imaging in this low-risk population of patients is rarely helpful and may generally be avoided, although careful clinical follow-up is warranted. Patients with HA-SAB who have mechanical valves, intracardiac devices, prolonged bacteremia or dialysis dependency have a high incidence of IE and should be evaluated thoroughly using echocardiography.

Similar content being viewed by others
References
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB (2004) Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infec Dis 39(3):309–317
Pien BC, Sundaram P, Raoof N, Costa SF, Mirrett S, Woods CW, Reller LB, Weinstein MP (2010) The clinical and prognostic importance of positive blood cultures in adults. Am J Med 123(9):819–828
Turnidge JD, Kotsanas D, Munckhof W, Roberts S, Bennet CM, Nimmo GR, Coomb GW, Murray RJ, Howden B, Johnson PD, Dowling K (2009) Staphylococcus aureus bacteraemia: a major cause of mortality in Australia and New Zealand. Med J Aust 191(7):368–373
Nadji G, Remadi JP, Coviaux F, Mirode AA, Brahim A, Enriquez-Sarano M, Tribouilloy C (2005) Comparison of clinical and morphological characteristics of Staphylococcus aureus endocarditis with endocarditis caused by other pathogens. Heart 91(7):932–937
Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, Bashore T, Corey GR (2000) Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 30(4):633–638
Durack DT, Lukes AS, Bright DK (1994) New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke endocarditis service. Am J Med 96(3):200–209
Gould FK, Denning DW, Elliott TS, Foweraker J, Perry JD, Prendergast BD, Sandoe JAT, Spry MJ, Watkin RW (2012) Guidelines for the diagnosis and antibiotic treatment of endocarditis in adults: a report of the Working Party of the British Society for antimicrobial chemotherapy. J Antimicrob Chemother 67:269–289
Baddour LM, Wilson WR, Bayer AS, Fowler VG Jr, Bolger AF, Levison ME, Ferrieri P, Gerber MA, Tani LY, Gewitz MH, Tong DC, Steckelberg JM, Baltimore RS, Shulman ST, Burns JC, Falace DA, Newburger JW, Pallasch TJ, Takahashi M, Taubert KA (2005) Infective endocarditis: diagnosis, antimicrobial therapy, and management of complications: a statement for healthcare professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association: endorsed by the Infectious Diseases Society of America. Circulation 111(23):e394–e434
Hilberath JN, Oakes DA, Shernan SK, Bulwer BE, D’Ambra MN, Eltzschig HK (2010) Safety of transesophageal echocardiography. J Am Soc Echocardiogr 23(11):1115–1127, quiz 220–221
Chang FY, MacDonald BB, Peacock JE Jr, Musher DM, Triplett P, Mylotte JM, O’Donnell A, Wagener MM, Yu VL (2003) A prospective multicenter study of Staphylococcus aureus bacteremia: incidence of endocarditis, risk factors for mortality, and clinical impact of methicillin resistance. Medicine 82(5):322–332
Fowler VG Jr, Olsen MK, Corey GR, Woods CW, Cabell CH, Reller LB, Cheng AC, Dudley T, Oddone EZ (2003) Clinical identifiers of complicated Staphylococcus aureus bacteremia. Arch Intern Med 163(17):2066–2072
Nickerson EK, Hongsuwan M, Limmathurotsakul D, Wuthiekanun V, Shah KR, Srisomang P, Mahavanakul W, Wacharaprechasgul T, Fowler VG Jr, West TE, Teerawatanasuk N, Becher H, White NJ, Chierakul W, Day NP, Peacock SJ (2009) Staphylococcus aureus bacteraemia in a tropical setting: patient outcome and impact of antibiotic resistance. PLoS One 4(1):e4308
Joseph JP, Meddows TR, Webster DP, Newton JD, Myerson SG, Prendergast B, Scarborough M, Herring N (2013) Prioritizing echocardiography in Staphylococcus aureus bacteraemia. J Antimicrob Chemother 68(2):444–449
Lautenschlager S, Herzog C, Zimmerli W (1993) Course and outcome of bacteremia due to Staphylococcus aureus: evaluation of different clinical case definitions. Clin Infec Dis 16(4):567–573
Kaasch AJ, Fowler VG Jr, Rieg S, Peyerl-Hoffmann G, Birkholz H, Hellmich M, Kern WV, Seifert H (2011) Use of a simple criteria set for guiding echocardiography in nosocomial Staphylococcus aureus bacteremia. Clin Infec Dis 53(1):1–9
Habib G, Hoen B, Tornos P, Thuny F, Prendergast B, Vilacosta I, Moreillon P, de Jesus AM, Thilen U, Lekakis J, Lengyel M, Müller L, Naber CK, Nihoyannopoulos P, Moritz A, Zamorano JL (2009) Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the task force on the prevention, diagnosis, and treatment of infective endocarditis of the European Society of Cardiology (ESC). Endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the International Society of Chemotherapy (ISC) for infection and cancer. Eur Heart J 30(19):2369–2413
Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, Nihoyannopoulos P, Otto CM, Quinones MA, Rakowski H, Stewart WJ, Waggoner A, Weissman NJ (2003) Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr 16(7):777–802
Khatib R, Sharma M (2013) Echocardiography is dispensable in uncomplicated Staphylococcus aureus bacteremia. Medicine 92(3):182–188
Holden E, Bashir A, Das I, Morton H, Steadman CD, Nightingale P, Steeds RP, David MD (2014) Staphylococcus aureus bacteraemia in a UK tertiary referral centre: a ‘transoesophageal echocardiogram for all’ policy. J Antimicrob Chemother 69(7):1960–1965
Barton TL, Mottram PM, Stuart RL, Cameron JD, Moir S (2014) Transthoracic echocardiography is still useful in the initial evaluation of suspected endocarditis. Mayo Clin Proc 89(6):799–805
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was obtained from any source for this project.
Conflict of interest
The authors report no financial conflicts or interests.
Rights and permissions
About this article
Cite this article
Barton, T., Moir, S., Rehmani, H. et al. Low rates of endocarditis in healthcare-associated Staphylococcus aureus bacteremia suggest that echocardiography might not always be required. Eur J Clin Microbiol Infect Dis 35, 49–55 (2016). https://doi.org/10.1007/s10096-015-2505-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-015-2505-8