Abstract
Purpose
Cardiac dysfunction risk associated with intravenous trastuzumab (H IV) treatment may differ in real-world practice versus randomized trials. We investigated cardiac events in patients with HER2-positive early breast cancer (EBC) treated with H IV as adjuvant therapy in routine practice.
Methods
The observational study of cardiac events in patients with HER2-positive EBC treated with Herceptin (OHERA; NCT01152606) enrolled patients with stage I–IIIb disease eligible for H IV in the adjuvant setting per the European Summary of Product Characteristics (SmPC). Primary outcomes were symptomatic congestive heart failure incidence (CHF; New York Heart Association class II–IV) and cardiac death. Patient visits/assessments were per local practice.
Results
3733 Patients received ≥ 1 H IV dose per local practice; 88.9% received H IV for > 300 days (median follow-up: ~ 5 years). Prior to disease recurrence (if any), symptomatic CHF occurred in 106 patients (2.8%); 6 (0.2%) cardiac deaths occurred (5 in patients with cardiac disease history). Median time to symptomatic CHF onset was 5.7 months (95% CI 5.3–6.5); 77/106 (72.6%) patients with symptomatic CHF achieved resolution. CHF incidence was higher in patients ≥ 65 years, and those with pre-existing cardiac conditions, hypertension, or left ventricular ejection fraction ≤ 55% at baseline.
Conclusions
OHERA is the largest prospective observational study to investigate the cardiac safety of H IV as adjuvant EBC therapy in a real-world setting. Symptomatic CHF and cardiac event incidences were consistent with randomized trials in this setting and baseline risk factors identified in the H IV European SmPC.
Similar content being viewed by others
Introduction
As of September 2018, > 2.7 million patients with breast cancer had received intravenous or subcutaneous trastuzumab (Herceptin®, F. Hoffmann-La Roche Ltd., Basel, Switzerland; intravenous trastuzumab (H IV) and subcutaneous trastuzumab (H SC), respectively) in clinical trial or real-world settings (Roche internal data).
The phase 3 HERceptin Adjuvant [HERA; Breast International Group (BIG) 01-01], National Surgical Adjuvant Breast and Bowel Project (NSABP)-B31/N9831, and Breast Cancer International Research Group (BCIRG)-006 studies demonstrated the clinical benefits of 1 year of H IV as adjuvant therapy for the treatment of patients with HER2-positive early breast cancer (EBC) [1,2,3]. H IV was approved for the treatment of HER2-positive EBC in the adjuvant setting in Europe, and many other countries worldwide, on the basis of significant improvements in disease-free survival (DFS) after 1 year, per the primary analysis of the HERA study (unadjusted hazard ratio for DFS 0.54 [95% confidence interval (CI) 0.44–0.67]; P < 0.0001) [1, 4]. Subsequent analyses of HERA, based on median follow-up periods of up to 11 years, reinforced the DFS benefits associated with 1 year of H IV treatment [1, 5,6,7] and overall survival was shown to be prolonged in patients who received H IV, compared with control arms, in long-term analyses from each of the three H IV adjuvant EBC studies [3, 5, 7, 8].
Anti-HER2 treatment is associated with increased risk of cardiac dysfunction, and particularly congestive heart failure (CHF) [1, 3, 4]. Risk of cardiac failure in H IV-treated patients is relevant in real-world clinical practice and may differ from the risk observed in a randomized, controlled clinical trial setting with strict entry criteria and follow-up procedures. Despite the increased risk of cardiac dysfunction associated with H IV in patients with breast cancer, the incidence of symptomatic CHF and significant decreases in left ventricular ejection fraction (LVEF) were low (1.7 and 7.1%, respectively) in the HERA study at 1-year median follow-up, and remained low during subsequent longer-term follow-up analyses (1.9 and 9.8%, respectively after a median follow-up of 3.6 years) [1, 9]. Moreover, long-term analyses of adjuvant EBC trials have suggested the majority of cardiac events are reversible [10, 11].
The present observational study of cardiac events in patients with HER2-positive EBC treated with Herceptin (OHERA; NCT01152606) was conducted as a post-authorization commitment following European Union (EU) approval of H IV in the adjuvant EBC setting. OHERA is a non-interventional, single-cohort safety study designed to investigate the incidence of cardiac events in a real-world population of patients with HER2-positive EBC being treated with H IV in the adjuvant setting as per the EU Summary of Product Characteristics (SmPC) [4], in routine clinical practice.
Here we report the final analysis of the OHERA study. The primary objective of the OHERA study was to observe, in the routine clinical practice setting, the incidence of symptomatic CHF and cardiac death in patients with HER2-positive EBC who received H IV per the approved EU SmPC. Secondary objectives were to explore potential risk factors for symptomatic CHF and cardiac death, to observe the time to onset and resolution of symptomatic CHF and other significant cardiac conditions, and to record the incidence of asymptomatic left ventricular dysfunction.
Methods
Study design
Patients with HER2-positive EBC (stage I–IIIb) being considered for treatment with H IV in the adjuvant setting per the EU SmPC were enrolled, treated, and monitored according to local practice [4]. No additional procedures/patient visits outside routine clinical practice were performed during the study. The study was conducted in accordance with the Declaration of Helsinki and the laws and regulations of each country in which the study was performed. The study protocol was approved by the Independent Ethics Committee or Institutional Review Board for each site prior to starting the study. Eligible patients were required to provide written informed consent prior to enrollment.
Patients
Due to the non-interventional nature of the study, no specific inclusion or exclusion criteria beyond the indication and contraindications in the H IV EU SmPC were applied when enrolling patients [4]. Patients with HER2-positive EBC whose tumors had either HER2 overexpression or HER2 gene amplification as determined by an accurate and validated assay were considered to be eligible for enrollment and treatment with H IV per the EU SmPC [4]. Patients with contraindications to H IV per the EU SmPC, i.e., those with known hypersensitivity to H IV, murine proteins, or any of the excipients, and patients with severe dyspnea at rest due to complications of advanced malignancy, or requiring supplementary oxygen therapy [4], were not eligible for this study.
Consenting patients were enrolled into the study sequentially without any pre-selection process, and irrespective of whether they subsequently received H IV following physician assessment of the benefit:risk balance.
Treatment with H IV was administered per local practice and in accordance with the EU SmPC. At study initiation in 2007, the approved treatment regimen in the EU SmPC for H IV as adjuvant therapy for HER2-positive EBC was monotherapy following surgery, chemotherapy, and/or radiotherapy based on the phase 3 HERA study results; subsequently in 2011, during the course of the OHERA study, approved treatment regimens in the EU SmPC were updated to include concurrent use of H IV with chemotherapy in the adjuvant treatment of patients with HER2-positive EBC as part of a treatment regimen consisting of doxorubicin and cyclophosphamide followed by H IV plus paclitaxel (PTX) or docetaxel, or H IV plus docetaxel plus carboplatin [4].
Outcomes
The primary safety outcomes were incidence of symptomatic CHF [New York Heart Association (NYHA) class II–IV] and incidence of cardiac death. Secondary outcomes included time to onset and time to recovery of symptomatic CHF and other cardiac conditions, and incidence of asymptomatic left ventricular dysfunction (evaluated as the incidence of significant LVEF drop; defined as at least one drop in LVEF of ≥ 10 percentage points from baseline to < 50%). Exploratory analyses of potential risk factors associated with incidence of symptomatic CHF were also conducted.
Assessments
Cardiac assessments were to be performed per local practice and/or in accordance with guidance contained in the approved H IV EU SmPC, which recommends LVEF assessments be performed at the time of treatment initiation (baseline), every 3 months during treatment, and at 6, 12, and 24 months after treatment discontinuation (exact schedules varied according to local practice). The frequency of LVEF assessments could be increased if clinically indicated, e.g., in cases of LVEF drop or presence of symptoms of cardiac dysfunction. Cardiac function and LVEF were monitored by echocardiogram (ECHO), multiple-gated acquisition (MUGA) scan, magnetic resonance imaging, or other methods per local practice. Data were collected on baseline demographics, breast cancer disease characteristics, medical history and pre-existing conditions ongoing at baseline (focusing on cardiac-related conditions and potential risk factors for cardiac events such as hypertension, diabetes mellitus, obesity, smoking habits, ischemic heart disease, or arrhythmias), previous anticancer therapy (and concurrent treatments if still ongoing at the time of starting H IV), hormonal therapy, radiotherapy treatment, and disease recurrence.
Patient data were to be collected for up to 5 years after the first H IV administration, or until death, loss to follow-up or withdrawal of consent, whichever occurred first.
Statistical analysis
As this study was not hypothesis testing, no formal sample size calculation was performed and all analyses are descriptive. However, a target enrollment of approximately 3800 patients treated with H IV was agreed with the European health authorities and considered sufficient to detect a 1% increase in CHF based on the background incidence of up to 4%, as reported in previous adjuvant EBC trials [2]. With the target enrollment of 3800 patients, the width of the Pearson–Clopper 95% CI remained reasonably small when assuming incidence rates ranging from 2% (95% CI 1.58–2.50) to 5% (95% CI 4.33–5.74).
The final analysis was conducted in the safety population, defined as all enrolled patients with EBC (stage I–IIIb) who received at least one dose of H IV in the adjuvant setting.
Demographic and baseline characteristic data were summarized for all patients in the safety population. CHF and cardiac death were summarized as incidence with two-sided Pearson–Clopper 95% CI. Only cardiac events and LVEF assessments prior to disease recurrence were included in the analyses. Time to event onset and resolution were analyzed using Kaplan–Meier methodology.
Results
In total, 3938 patients were enrolled between August 2007 and November 2010 at 199 sites across Austria, Belgium, Germany, Hungary, Italy, Poland, Spain, Sweden, and the UK. Of these, 3733 (95%) individuals had stage I–IIIb breast cancer and received at least one dose of study treatment, and therefore comprised the safety population (Fig. 1). The median age of patients in the safety population was 55.0 years (range 21–86 years; Table 1) and > 99% of patients were women. The majority of patients (> 80%) had stage I or II breast cancer, 62.6% were estrogen receptor-positive, and 90.2% had received prior anthracycline-based chemotherapy before starting H IV treatment (Table 1). Concurrent medications are provided in Supplementary Table 1. The median LVEF at baseline was 64.0 (range 36–90) and 356 (9.5%) patients had a family history of CHF. Overall, 1574 (42.2%) patients had ≥ 1 pre-existing cardiovascular medical condition representing a risk for symptomatic CHF including hypertension (28.3%), thyroid gland disorder (10.4%), dyslipidemia (7.5%), and diabetes mellitus (4.7%) (Table 1); 1143 patients (30.6%) were current or ex-smokers.
Overall, 799 (21%) patients withdrew from the study prematurely. Reasons for premature withdrawal included death (n = 263), loss to follow-up (n = 373), withdrawal of consent (n = 55), or admin/other reasons (n = 108).
The median duration of follow-up was approximately 5.0 years (1829 days, interquartile range 1793–1867 days).
H IV treatment characteristics
The median duration of H IV adjuvant EBC treatment in the safety population was 11.8 months, and 88.9% (n = 3318) of patients were treated for > 300 days. A small number of patients (78 [2.1%]) had a total treatment duration of > 420 days, most likely due to treatment delays or interruptions.
Patients who experienced symptomatic CHF during the study had shorter median treatment duration and reduced treatment exposure as compared with those who did not have CHF during the study (median treatment duration 6.4 vs. 11.8 months; median cumulative dose 4117 vs 7080 mg, respectively).
Incidence of symptomatic CHF and cardiac death
Symptomatic CHF (NYHA class II–IV) was reported in 106 (2.8%) patients, 91.5% (97/106) of whom received at least one treatment for CHF. Resolution of symptomatic CHF was achieved in 72.6% (77/106) of these individuals (as per the treating physician’s assessment) (Table 2). The most common treatments prescribed for the treatment of CHF included β-adrenoreceptor-blocking agents, angiotensin-converting enzyme inhibitors, and diuretics.
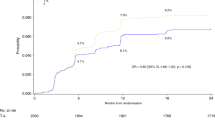
The median time to onset of symptomatic CHF was 5.7 months (95% CI 5.3–6.5; Fig. 2) and the median time from onset to resolution was 9.9 months (95% CI 8.3–13.6).
Severe CHF (NYHA class III or IV) occurred in 38 (1.0%) patients and cardiac death occurred in 6 (0.2%) (Table 2). Five of the six patients who experienced cardiac death had a previous history of cardiovascular disease. The median time to cardiac death was 4.3 years (range 0.2–4.8).
In total, 264 patients died during the full study period (including deaths that occurred after disease recurrence). Of the deaths reported, 205 were related to metastases or disease progression, 14 were attributed to other cancers (cervical, ovarian, bladder, pancreatic, gastrointestinal, leukemia, glioblastoma, renal cancer, and neoplasm), and 11 were cardiac deaths.
Incidence and resolution of significant LVEF drop
A significant drop in LVEF was observed in 251/3291 patients (7.6%), among whom resolution was documented in 169 (67.3%) (Table 2). The median time to onset of significant LVEF drop was 6.6 months (95% CI 5.8–7.2); and the median time from onset to resolution of LVEF drop was 8.8 months (95% CI 5.7–13.6).
The median LVEF was approximately 60% at baseline in patients who experienced symptomatic CHF. In these patients, LVEF generally decreased during the first 3 months after initiation of H IV, was lowest during Months 4–9, before stabilizing above 50% during Months 13–18 (Supplementary Fig. 1).
Additional cardiac adverse events
In total, 652 (17.5%) patients experienced cardiac adverse events (AEs) prior to disease recurrence that were not classified as symptomatic CHF (individual events summarized in Table 3). When considering only the highest-grade AE experienced by an individual patient, most non-CHF cardiac AEs were Grade 1 (7.5%, 280 patients) or Grade 2 (7.1%, 264 patients). The overall incidence of Grade 3 or higher non-CHF cardiac events was low; incidence of Grade 3, 4, and 5 events was 2.4% (90 patients); 0.3% (11 patients), and 0.2% (6 patients), respectively.
Baseline risk factors associated with increased incidence of CHF
The incidence of CHF was higher in patients with the following baseline characteristics: pre-existing cardiac conditions, use of cardiovascular medications, hypertension, LVEF ≤ 55%, body mass index (BMI) ≥ 25 kg/m2, age ≥ 65 years, family history of CHF or history of cardiac failure at study entry, and history of CHF or diagnosis of CHF active at study entry (Fig. 3). The incidence of CHF was not higher in patients who had received prior anthracycline therapy at baseline or in those who had received prior left-side radiotherapy. Although the incidence of CHF in OHERA was increased in patients with LVEF ≤ 55%, the incidence of severe CHF in the overall population was consistent with the incidence observed in the HERA study, in which patients were required to have an LVEF ≥ 55% [1, 6, 9].
Discussion
The incidence rates of symptomatic CHF and cardiac death in the real-world population in the OHERA study were low and consistent with cardiac results from the HERA phase 3 randomized clinical trial (Supplementary Table 2) [1, 6, 7, 9]. Incidence of severe CHF in OHERA was also comparable with reports from the HERA study (1.0 vs. 0.5–0.8% [1], respectively) [1, 6, 9] and slightly lower than the incidence reported in most other adjuvant EBC trials (Supplementary Table 2) [3, 8, 12, 13]. The majority of patients treated per routine clinical practice in OHERA had an overall H IV treatment duration of approximately 1 year, consistent with the recommended treatment duration for EBC patients as described in the current H IV EU SmPC [4].
For most patients who experienced symptomatic CHF or significant LVEF drop in OHERA, the events began during treatment and resolved during the study period, suggesting that the cardiotoxicity associated with trastuzumab may be reversible, and that standard cardiac medications may lead to resolution of these cardiac events. This is consistent with data from HERA, which showed that the majority of patients recovered from non-fatal cardiac events including confirmed LVEF drop (recovery rate 83.3%), symptomatic CHF (recovery rate 78.1%), and severe CHF (recovery rate 69.2%) [9]. This is also consistent with the cardiac safety analyses of the other H IV adjuvant EBC trials, in which the majority of patients with cardiac events were recorded as having improved cardiac function during long-term follow-up analyses [3, 10, 11, 13, 14].
Importantly, patients were enrolled in OHERA according to the approved H IV EU SmPC and local practice, and approximately 10% of the patients in OHERA had an LVEF ≤ 55% at baseline; whereas, the HERA study enrolled only women with a baseline LVEF of ≥ 55% after completing chemotherapy or radiotherapy. Nevertheless, cardiac events in OHERA were consistent with that observed in the HERA study. Differences observed in the incidence of significant LVEF drops in OHERA (7.6%) compared to HERA (from 3.6% confirmed to 9.8% unconfirmed) [9], and as reported in other H IV EBC studies (Supplementary Table 2) are likely influenced by different study definitions for ‘significant’ LVEF drops and different follow-up periods.
Previous observational studies have reported rates of H IV-related cardiotoxicity (including both asymptomatic and symptomatic cardiac events) ranging from 15 to 27% [15,16,17]. Additionally, retrospective studies conducted in Israel and the US have reported cardiotoxicity/cardiac event rates ranging from 21 to 29% [18,19,20]. A recent population-based cohort study, including 4082 H IV-treated patients with breast cancer and a median age between 52 and 58 years [21], depending on the chemotherapy partner received reported higher cumulative incidence rates of cardiotoxicity following trastuzumab therapy than have been reported in previous clinical trials. These differences reflect variation in the definition of endpoints, duration of follow-up, and the characteristics of patients included in these analyses, all of which make cross-study comparisons challenging both between real-world studies and with randomized controlled trials. Real-world analyses conducted in restricted geographic regions are also likely to be influenced by regional differences in clinical practice, such as the use of radiotherapy and anthracyclines (although it should be noted that over 90% of patients in OHERA had received prior anthracycline therapy) [16, 20]. The prevalence of recognized risk factors for cardiotoxicity in different study populations is also important. For example, the increased rates of cardiac events reported in two large retrospective studies in the US may at least partially relate to those studies focusing on elderly patients (mean age 76 years [19] and median age 71 years in the overall population [including patients not treated with H IV]) [18], vs. median age 55 years in OHERA, a demographic group commonly underrepresented in clinical trials and also recognized as at increased risk for cardiotoxicity [4, 18, 19]. In addition, most cardiac events are reported to be reversible in observational studies and long-term follow-up analyses of the H IV adjuvant EBC trials [6, 11, 15,16,17].
The incidence of CHF in OHERA was low overall, but higher in selected subgroups including patients with recognized cardiac conditions at baseline, older patients (< 65 vs. ≥ 65 years), and patients with lower baseline LVEF (≤ 55% vs. > 55%). These observations are consistent with the results of NSABP-31, which showed that the relative risk of CHF increases significantly with age and with impairment in LVEF either at baseline or at the end of chemotherapy (doxorubicin plus cyclophosphamide) [13]. In particular, data from NSABP-31 showed that the risk of CHF increased significantly in patients aged 50–59 and ≥ 60 years relative to those aged < 50 years, and in patient subgroups with a baseline LVEF of 50–54% versus those with an LVEF of 55–64 and ≥ 65% [13]. Thus, relatively small differences in age or baseline LVEF may be associated with increases in the risk of CHF and may explain differences in CHF incidence between studies. Interestingly, the incidence of CHF was not higher in patients who had received left-side radiotherapy at baseline in OHERA, compared with those who did not.
The potential impact of treatment regimens comprising H IV plus anthracyclines on cardiotoxicity rates was demonstrated in a Chinese observational study, which reported that patients with EBC who received H IV plus anthracyclines, had a higher rate of cardiotoxicity than that observed in patients who received H IV without anthracyclines [16]. This association of cardiotoxicity between H IV and patients who received baseline anthracyclines was not seen in OHERA, and may have been due to clinical factors that allowed patients to receive baseline anthracyclines.
In summary, our data support previous reports that the majority of cardiac events are asymptomatic or mild and that the rates of severe or refractory CHF in patients treated with H IV are low in real-world populations [16, 17, 22].
This study has potential limitations, in addition to those intrinsic to its observational, non-interventional nature. Since patients were selected for treatment with H IV in accordance with the EU SmPC, this may have resulted in the selection of patients with different baseline characteristics compared with those in previous trastuzumab randomized clinical trials in EBC. Subjective assessment of the risk of cardiotoxicity associated with H IV by the patient or physician may have led to inadvertent selection of patients according to prognosis (channeling bias) [23]. Due to the non-interventional nature of the study, there was increased potential for patients to miss an LVEF assessment. Resolution of symptomatic CHF was defined by the treating physician and the exact definition of resolution could have differed between physicians. Importantly, recruitment of patients in OHERA was guided by indications in the EU SmPC at the time the study was initiated. Thus, although this study provides strong data on cardiac risks in a patient population treated with H IV as adjuvant EBC therapy in routine clinical practice, the study population differs from those in previous randomized controlled trials and observational studies, limiting the direct comparability of our results.
In conclusion, OHERA is the largest prospective observational study (> 3700 treated patients) to date to investigate the cardiac safety of H IV as adjuvant EBC therapy in a real-world patient population. The study’s final results are consistent with cardiac safety data reported in previous clinical trials that evaluated H IV treatment in the adjuvant setting for HER2-positive EBC [1, 2, 5,6,7, 9], such as the HERA study [1], and are consistent with the baseline risk factors for CHF as reported in the EU H IV SmPC [4].
Data Availability
Qualified researchers may request access to individual patient-level data through the clinical study data request platform (http://www.clinicalstudydatarequest.com). Further details on Roche's criteria for eligible studies are available here (https://clinicalstudydatarequest.com/Study-Sponsors/Study-Sponsors-Roche.aspx). For further details on Roche's Global Policy on the Sharing of Clinical Information and how to request access to related clinical study documents, see here (https://www.roche.com/research_and_development/who_we_are_how_we_work/clinical_trials/our_commitment_to_data_sharing.htm).
Abbreviations
- AC-T:
-
Doxorubicin and cyclophosphamide followed by docetaxel
- AE:
-
Adverse event
- BCIRG:
-
Breast Cancer International Research Group
- BIG:
-
Breast International Group
- BMI:
-
Body mass index
- CHF:
-
Congestive heart failure
- CI:
-
Confidence interval
- DFS:
-
Disease-free survival
- EBC:
-
Early breast cancer
- ECHO:
-
Echocardiogram
- H IV:
-
Intravenous trastuzumab
- H SC:
-
Subcutaneous trastuzumab
- LVEF:
-
Left ventricular ejection fraction
- MUGA:
-
Multiple-gated acquisition
- NCI-CTCAE:
-
National Cancer Institute-Common Terminology Criteria for Adverse Events
- NSABP:
-
National Surgical Adjuvant Breast and Bowel Project
- NYHA:
-
New York Heart Association
- PTX:
-
Paclitaxel
- SmPC:
-
Summary of Product Characteristics
References
Piccart-Gebhart MJ, Procter M, Leyland-Jones B et al (2005) Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med 353:1659–1672. https://doi.org/10.1056/NEJMoa052306
Romond EH, Perez EA, Bryant J et al (2005) Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med 353:1673–1684. https://doi.org/10.1056/NEJMoa052122
Slamon D, Eiermann W, Robert N et al (2011) Adjuvant trastuzumab in HER2-positive breast cancer. N Engl J Med 365:1273–1283. https://doi.org/10.1056/NEJMoa0910383
Roche Registration Ltd. Herceptin® (trastuzumab). Summary of product characteristics. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000278/WC500074922.pdf. Accessed Sep 2018
Cameron D, Piccart-Gebhart MJ, Gelber RD et al (2017) 11 Years’ follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive early breast cancer: final analysis of the HERceptin Adjuvant (HERA) trial. Lancet 389:1195–1205. https://doi.org/10.1016/S0140-6736(16)32616-2
Goldhirsch A, Gelber RD, Piccart-Gebhart MJ et al (2013) 2 Years versus 1 year of adjuvant trastuzumab for HER2-positive breast cancer (HERA): an open-label, randomised controlled trial. Lancet 382:1021–1028. https://doi.org/10.1016/S0140-6736(13)61094-6
Smith I, Procter M, Gelber RD et al (2007) 2-Year follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer: a randomised controlled trial. Lancet 369:29–36. https://doi.org/10.1016/S0140-6736(07)60028-2
Perez EA, Romond EH, Suman VJ et al (2011) Four-year follow-up of trastuzumab plus adjuvant chemotherapy for operable human epidermal growth factor receptor 2-positive breast cancer: joint analysis of data from NCCTG N9831 and NSABP B-31. J Clin Oncol 29:3366–3373. https://doi.org/10.1200/JCO.2011.35.0868
Procter M, Suter TM, de Azambuja E et al (2010) Longer-term assessment of trastuzumab-related cardiac adverse events in the Herceptin Adjuvant (HERA) trial. J Clin Oncol 28:3422–3428. https://doi.org/10.1200/JCO.2009.26.0463
Advani PP, Ballman KV, Dockter TJ et al (2016) Long-term cardiac safety analysis of NCCTG N9831 (Alliance) adjuvant trastuzumab trial. J Clin Oncol 34:581–587. https://doi.org/10.1200/JCO.2015.61.8413
de Azambuja E, Procter MJ, van Veldhuisen DJ et al (2014) Trastuzumab-associated cardiac events at 8 years of median follow-up in the Herceptin Adjuvant trial (BIG 1-01). J Clin Oncol 32:2159–2165. https://doi.org/10.1200/JCO.2013.53.9288
Romond EH, Jeong JH, Rastogi P et al (2012) Seven-year follow-up assessment of cardiac function in NSABP B-31, a randomized trial comparing doxorubicin and cyclophosphamide followed by paclitaxel (ACP) with ACP plus trastuzumab as adjuvant therapy for patients with node-positive, human epidermal growth factor receptor 2-positive breast cancer. J Clin Oncol 30:3792–3799. https://doi.org/10.1200/JCO.2011.40.0010
Tan-Chiu E, Yothers G, Romond E et al (2005) Assessment of cardiac dysfunction in a randomized trial comparing doxorubicin and cyclophosphamide followed by paclitaxel, with or without trastuzumab as adjuvant therapy in node-positive, human epidermal growth factor receptor 2-overexpressing breast cancer: NSABP B-31. J Clin Oncol 23:7811–7819. https://doi.org/10.1200/JCO.2005.02.4091
Perez EA, Suman VJ, Davidson NE et al (2008) Cardiac safety analysis of doxorubicin and cyclophosphamide followed by paclitaxel with or without trastuzumab in the North Central Cancer Treatment Group N9831 adjuvant breast cancer trial. J Clin Oncol 26:1231–1238. https://doi.org/10.1200/JCO.2007.13.5467
Tarantini L, Cioffi G, Gori S et al (2012) Trastuzumab adjuvant chemotherapy and cardiotoxicity in real-world women with breast cancer. J Card Fail 18:113–119. https://doi.org/10.1016/j.cardfail.2011.10.015
Xue J, Jiang Z, Qi F et al (2014) Risk of trastuzumab-related cardiotoxicity in early breast cancer patients: a prospective observational study. J Breast Cancer 17:363–369. https://doi.org/10.4048/jbc.2014.17.4.363
McArthur HL, Chia S (2007) Cardiotoxicity of trastuzumab in clinical practice. N Engl J Med 357:94–95. https://doi.org/10.1056/NEJMc070065
Chavez-MacGregor M, Zhang N, Buchholz TA et al (2013) Trastuzumab-related cardiotoxicity among older patients with breast cancer. J Clin Oncol 31:4222–4228. https://doi.org/10.1200/JCO.2013.48.7884
Chen J, Long JB, Hurria A et al (2012) Incidence of heart failure or cardiomyopathy after adjuvant trastuzumab therapy for breast cancer. J Am Coll Cardiol 60:2504–2512. https://doi.org/10.1016/j.jacc.2012.07.068
Fried G, Regev T, Moskovitz M (2013) Trastuzumab-related cardiac events in the treatment of early breast cancer. Breast Cancer Res Treat 142:1–7. https://doi.org/10.1007/s10549-013-2732-6
Thavendiranathan P, Abdel-Qadir H, Fischer HD et al (2016) Breast cancer therapy-related cardiac dysfunction in adult women treated in routine clinical practice: a population-based cohort study. J Clin Oncol 34:2239–2246. https://doi.org/10.1200/JCO.2015.65.1505
Tarantini L, Gori S, Faggiano P et al (2012) Adjuvant trastuzumab cardiotoxicity in patients over 60 years of age with early breast cancer: a multicenter cohort analysis. Ann Oncol 23:3058–3063. https://doi.org/10.1093/annonc/mds127
Petri H, Urquhart J (1991) Channeling bias in the interpretation of drug effects. Stat Med 10:577–581. https://doi.org/10.1002/sim.4780100409
Acknowledgements
We would like to thank the patients, their families, the nurses, and the investigators who participated in this study.
Funding
The OHERA study was sponsored by F. Hoffmann-La Roche Ltd., Basel, Switzerland. Support for third-party writing assistance for this manuscript, furnished by Rachel Johnson, PhD, of Health Interactions, was provided by F. Hoffmann-La Roche Ltd., Basel, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The OHERA study was sponsored by F. Hoffmann-La Roche Ltd., Basel, Switzerland. Dr. Lidbrink reports Consultancy/Advisory role for F. Hoffmann-La Roche. Dr. Chmielowska reports research funding from F. Hoffmann-La Roche. Dr. Bouhlel, Mr. Liste Hermoso, and Dr. Nüesch are employees of F. Hoffmann-La Roche Ltd. Dr. Bouhlel and Dr. Nüesch report stock in F. Hoffmann-La Roche Ltd. Dr. Lauer reports consultancy for F. Hoffmann-La Roche Ltd. Dr. Shing was an employee of Genentech, Inc., at the time of this study and reports remuneration and consultancy for Genentech, Inc. Dr. Misra reports Consultancy/Advisory role for Eisai, Amgen, and Pfizer. Dr. Otremba reports no financial conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the Ethical Standards of the Institutional and/or National Research Committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Dr. M. Shing was an employee of Genentech, Inc. at the time of this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Lidbrink, E., Chmielowska, E., Otremba, B. et al. A real-world study of cardiac events in > 3700 patients with HER2-positive early breast cancer treated with trastuzumab: final analysis of the OHERA study. Breast Cancer Res Treat 174, 187–196 (2019). https://doi.org/10.1007/s10549-018-5058-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-018-5058-6