Abstract
Background
In 2012, nearly one-third of adults 65 years or older with Medicare discharged to home after hospitalization were referred for home health care (HHC) services. Care coordination between the hospital and HHC is frequently inadequate and may contribute to medication errors and readmissions. Insights from HHC nurses could inform improvements to care coordination.
Objective
To describe HHC nurse perspectives about challenges and solutions to coordinating care for recently discharged patients.
Design/Participants
We conducted a descriptive qualitative study with six focus groups of HHC nurses and staff (n = 56) recruited from six agencies in Colorado. Focus groups were recorded, transcribed, and analyzed using a mixed deductive/inductive approach to theme analysis with a team-based iterative method.
Key Results
HHC nurses described challenges and solutions within domains of Accountability, Communication, Assessing Needs & Goals, and Medication Management. One additional domain of Safety, for both patients and HHC nurses, emerged from the analysis. Within each domain, solutions for improving care coordination included the following: 1) Accountability—hospital physicians willing to manage HHC orders until primary care follow-up, potential legislation allowing physician assistants and nurse practitioners to write HHC orders; 2) Communication—enhanced access to hospital records and direct telephone lines for HHC; 3) Assessing Needs & Goals—liaisons from HHC agencies meeting with patients in hospital; 4) Medication Management—HHC coordinating directly with clinician or pharmacist to resolve discrepancies; and 5) Safety—HHC nurses contributing non-reimbursable services for patients, and ensuring that cognitive and behavioral health information is shared with HHC.
Conclusions
In an era of shared accountability for patient outcomes across settings, solutions for improving care coordination with HHC are needed. Efforts to improve care coordination with HHC should focus on clearly defining accountability for orders, enhanced communication, improved alignment of expectations for HHC between clinicians and patients, a focus on reducing medication discrepancies, and prioritizing safety for both patients and HHC nurses.
Similar content being viewed by others
INTRODUCTION
Over the past several years, home health care (HHC) referrals at hospital discharge have increased,1 which could be related to the emergence of readmissions penalties,2 alternative payment models that increase hospital accountability beyond discharge,3 and the growing number of older adults who need skilled HHC services after discharge.4 A majority of older patients referred for HHC at hospital discharge have Medicare insurance, which requires that patients meet the following three conditions for skilled HHC services to be reimbursable: 1) are under the care of a physician, 2) have a need for a skilled HHC service (e.g., nursing, physical therapy) certified by a physician, and 3) are homebound (e.g., have great difficulty leaving home due to a medical condition).5 , 6
Patients referred for HHC may be particularly vulnerable after hospital discharge, as they are nearly 3 years older, have one additional comorbidity, and have higher severity of illness than patients discharged home without HHC.5 Readmission rates for HHC patients are higher than the national average for high-risk conditions such as heart failure (HF), in which 30-day readmission rates for Medicare beneficiaries discharged with HHC are as high as 23–26%,7 , 8 compared to a 21.9% overall national average for Medicare patients discharged with HF.9
The high-risk characteristics of patients referred for HHC after hospital discharge and suboptimal communication between HHC and other clinicians may both contribute to readmissions from HHC. In a study of HHC nurses in Norway, participants identified insufficient information exchange and communication with clinicians in other settings as contributors to medication errors.10 In addition, communication failures between HHC nurses and physicians have been found to increase the probability of hospital readmission by nearly 10% in high-risk patients with HF who receive HHC at discharge.11
As a partner in the continuum of care, nurses provide a majority of HHC services and have a critical role in crafting and implementing a patient’s plan of care after discharge.12 , 13 An evaluation of Medicare home health practices found that nurses completed over 98% of the first HHC visits for Medicare patients.14 During the initial HHC visit, HHC nurses focus on assessing a patient’s functional status, symptoms, medications, and several additional aspects of care to complete the standard Outcome and Assessment Information Set, in addition to implementing physician orders for the start of care.15 The HHC nurse scope of practice includes standards related to coordination of care and communication, as well as collaboration with patients and other clinicians.16 Yet, despite the key role of HHC nurses in care transitions, little is known about nurse experiences in coordinating care with other clinicians.
In a prior qualitative study, we found that both hospitalists and primary care providers (PCPs) expressed reservations about managing HHC orders following discharge.17 In that study, hospitalists expressed the belief that once a patient was discharged, HHC was the PCP’s responsibility, yet PCPs described challenges in addressing HHC requests if they had not yet evaluated a patient after discharge. As a result, HHC clinicians may not receive orders or information needed to provide optimal transitional care for patients.18 Because HHC nurse insights could inform how to improve care coordination to avoid readmissions from HHC, we sought HHC nurse perspectives about challenges and solutions to coordinating care for recently discharged patients.
METHODS
Study Design
We conducted a descriptive qualitative study of HHC nurses and administrators recruited from HHC agencies in Colorado. Six focus groups were conducted from September 2015 through June 2016, and were moderated by one of two team members: a licensed social worker with health care experience (DL) and a nurse with HHC experience (AR). Informed consent and a written survey including questions about demographics, years in practice, agency characteristics (e.g., access to hospital EHR), and receipt of information from hospital (e.g., main contact for information) were completed by participants at the beginning of each session. Group discussions lasted an average of 59.5 min (range 56–61 min), and were digitally recorded and transcribed verbatim. This protocol was found to be exempt by the Colorado Multiple Institutional Review Board (15–1281).
Population
We used a purposeful sampling strategy to recruit HHC agencies who had an active referral relationship with our hospital and diverse characteristics (e.g., for profit vs. not for profit). We conducted focus groups within individual agencies because nurses who deliver care in the same agency likely have common experiences. We chose to focus on HHC nurses because they complete a vast majority of the initial HHC visits with patients, and therefore would have insights into coordinating care in the time immediately following hospital discharge.14
Leadership from seven home health agencies was initially approached by phone or email to determine interest in participation. Six agreed to participate, and one for-profit agency with a regional presence in Colorado did not respond. Within interested agencies, email invitations were sent by agency leadership to encourage nurses to participate in focus groups. We requested that leadership recruit 6–10 participants, with a maximum of 12 participants per group. This recruitment strategy did not allow systematic collection of information about those who did not participate in focus groups.
Framework
Domains selected from the Agency for Healthcare Research and Quality (AHRQ) Care Coordination Measurement Framework were mapped to interview guide questions (Online Appendix).19 This AHRQ framework was developed from a comprehensive review of care coordination measures from multiple perspectives, including patients, caregivers, and clinicians. We chose this framework due to its broad applicability to care coordination between individuals in different roles and settings. Domains were selected based on relevance for care transitions from the hospital to HHC, and were drawn from domains identified in prior research with hospitalists and PCPs.17 The AHRQ framework domains and definitions are as follows:
-
1)
Accountability: defining responsibility of clinicians for an aspect of a patient’s care
-
2)
Communication: sharing knowledge among clinicians participating in a patient’s care
-
3)
Assessing Needs & Goals: determining care needs and goals with input from the patient and clinicians caring for the patient
-
4)
Medication Management: reconciling medication lists to avoid discrepancies and adverse events19
Analysis
The analysis team (CDJ, JJ, AR, DL) used an inductive theme approach to identify commonly encountered challenges and solutions in care coordination, and deductively mapped these to the AHRQ framework domains.20 Two team members coded each transcript and resolved discrepancies through group discussion. Using a team-based iterative approach,21 , 22 the analysis team met after every 1–2 focus groups to ensure that content was building iteratively until we reached thematic saturation.23 Key discussion themes and preliminary results were shared with focus group representatives to perform member checks and re-contextualize the analysis team’s interpretations. Analysis was facilitated by ATLAS.ti, version 7.5.15 (Scientific Software Development GmbH, Berlin, Germany).
RESULTS
A total of 56 HHC nurses and administrators participated in six focus groups. Demographic and agency-level data are shown in Table 1. Most participants were women (93%), and 76% identified as HHC nurses. The 13 administrators held the following positions: four directors or branch managers, three nurse clinical managers, three home care coordinators, two clinical service directors, and one managed referrals and clinical oversight. Among HHC agencies, the number of full-time employees (e.g., nurses; physical, occupational, or speech therapists) ranged from 22 to over 100. Five of six HHC agencies were for-profit. Four were freestanding and two were part of a national chain. All were in the Denver metropolitan area, and all used EHRs in their practices to provide clinical care. Two agencies had access to the EHR of at least one referring hospital.
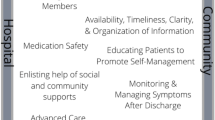
Participants discussed multiple themes which mapped to the framework domains of Accountability, Communication, Assessing Needs & Goals, and Medication Management. An additional domain of Safety in the home environment was identified during analysis. The relationship among the five domains is depicted in Figure 1. Themes within the Accountability and Communication domains were commonly in the context of HHC nurse-initiated interactions with hospital clinicians and PCPs. Both Accountability and Communication domains are included in the left-most circle to portray the lack of clarity about responsibility for these domains between hospital clinicians on the top and PCPs on the bottom. Themes within Assessing Needs & Goals were frequently in the context of attempts to coordinate care among the hospital clinician, PCP, and HHC nurses, hence its location in the middle of the figure. Themes within the Medication Management and Safety domains were commonly described as something that the HHC nurse navigates with the patient in the home. Results are organized by the five domains, with related themes presented as challenges and solutions (Table 2).
Accountability
The importance of physician accountability for HHC orders, and accountability related to payer requirements for physicians to write HHC orders, were key themes. Resistance from the hospital clinicians and staff to accountability for HHC is a frequently encountered challenge, as in the following quote:
As a general rule, I’ve been told you’re not to contact the hospitals. I actually got in trouble for contacting the hospital, trying to find out, get more information, trying to track a doctor down. I got in trouble for involving the hospital people… my experience is they don’t want us calling and trying to get more information from the hospital.
Participants described challenges related to caring for patients caught between hospital clinicians and staff resistant to taking responsibility after discharge, and a PCP lacking necessary information to assume responsibility for HHC orders:
Call a [PCP] on the weekend and they say ‘I know nothing…I didn’t know they were in the hospital. I don’t have a report on this patient’ even though it’s their patient... The communication between the hospital and the [PCPs] is just as bad as it is for us, because the PCPs don’t have the information.
However, finding hospital physicians willing to sign and manage HHC orders until a patient visits their PCP helps to overcome this challenge:
I had this stroke patient that has not established primary care yet and the primary care …said they would not sign or authorize home care to start until the patient came in and initially had the first visit, so the neuro floor doctor who saw the patient… actually agreed to follow home care until the patient establishes…
Another key theme related to accountability is an insurance requirement that only physicians can order HHC services. As a result, when a nurse practitioner (NP) provides primary care for a patient, obtaining HHC orders can be challenging:
[We have] big problems too with using the primary physician in some of the clinics… because most of the patients… see nurse practitioners and not a doctor and [insurance] requires us to have a physician’s order for care.
One participant expressed support for anticipated legislation allowing NPs and physician assistants (PAs) to sign HHC orders to address this accountability challenge:
We’re trying to change it though from national level…it’s on the legislative slate. It’s pretty much at the top. And we support it. We would love … to be able to accept [physician assistants’ and nurse practitioners’] orders for home health. We’re for it.
Communication
The ability for HHC nurses to provide optimal care following discharge often depends upon access to hospital records, and the ability to reach clinicians involved in the patient’s care. Lacking access to hospital records can lead to HHC encounters where important medical information is unknown, resulting in unmet patient needs:
…it’s super common for us to send [a HHC nurse] out, and they say ‘Oh, this patient has a wound. ‘ …we didn’t know they had a wound…and so we have no orders to put on a wound vac, but we have a wound vac there and we have a wife screaming at us that we have to put a wound vac on…
Enhanced access to a hospital’s EHR can improve HHC through increased knowledge about emergency department visits and hospitalizations. EHR access can also promote proactive communications from the hospital:
…[the hospital case managers] will automatically grant me access [to the hospital EHR]… so that we can see what’s going on and we can print the ER visit if the patient isn’t admitted…if the patient is being admitted, they put a note in... [HHC agency name] is following, so then I get a call from the floor asking for a report.
When participants encounter clinical questions, the challenge of connecting with a clinician, either from the hospital or primary care clinic, is a critical challenge to providing optimal HHC services. Although 63% (32 of 51) of participants indicated on the survey that hospital case managers or social workers were their main point of contact for information following discharge, often HHC nurses need a physician’s order or guidance. The frustration this creates for HHC nurses is reflected in the following quote:
Getting a hold of a physician is kind of a fruitless effort… we don’t get callbacks frequently…
On the other hand, a direct line to a clinician can facilitate communication to avoid unnecessary hospitalizations, as in this patient with cellulitis:
I actually got a hold of her PCP and she just extended her [antibiotics]. [The PCP] just called in a new prescription and avoided another probably unnecessary hospitalization…
Assessing Needs & Goals
Clinician understanding of HHC services is a key theme that emerged within the domain of Assessing Needs & Goals. Poor understanding of HHC services from both hospital clinicians and PCPs was discussed in nearly all groups as a contributor to unmet patient expectations with HHC.
One thing I’d say about the discharge process is the hospital not explaining to the patient what to expect from home health care…So it kind of sets an unfortunate expectation for us … and so the expectation at that time is shattered, you know, in the way [the patients are] viewing us, so then [we] have to rebuild this relationship.
However, liaisons from HHC agencies who meet with patients in the hospital to explain and coordinate HHC services can help to better align patient and HHC nurse expectations:
Optimally, as the liaison if you get the call before the hospital discharges the patients, you can come out, meet with the patient, get the records, get the orders… and let the patient know what the expectations are, this is who is going to see you, this is what your orders are for …and then the [HHC nurse] has that information on her device as she goes out to see the patient…
Medication Management
In most groups, participants described medication list discrepancies resulting from suboptimal communication and unclear accountability between clinicians in the hospital and clinic settings:
…most medication lists are incorrect because there’s multiple doctors involved... The list that you have doesn’t match what the patient has at home. The list that the primary doctor has doesn’t match the list that was in the hospital so, you know, it becomes a real sort of a knot that we have to untangle…
This lack of communication between medication prescribers in different settings can contribute to medication errors:
…it’s even more scary when they have a cardiologist and then a kidney specialist, and they’re all prescribing different meds… [the patient will] have atenolol and metoprolol… all these different kind of medications for the same thing by different doctors, and [the doctors] don’t know that the patient has that from another doctor so…it’s really scary.
However, coordinating directly with a PCP office or pharmacist can help resolve medication discrepancies:
[With the primary care office]…over the phone, we just went over every single medication and what the dosage was, how often [the patient was] supposed to take it and … it was so helpful ‘cause now [the patient] has an accurate med list in the home, she knows what she’s taking …
Safety
Safety in the home environment for patients and HHC nurses was a new domain that emerged during analysis. The patient experience of safety in their home is best understood by HHC nurses, but not always fully understood or communicated by hospital clinicians, particularly in the case of cognitive impairment:
I mean, we see many at home that maybe are living alone and there is some element of dementia …they may not have a lot of dementia on board, but always that transition … out of a facility back home again, there is a period of confusion. You see it all the time, you know, trying to transition, and it usually takes about a week and then they’re back into their environments…
Yet, patients often have a strong desire to stay at home, even in the context of ailing health:
[The patients] would rather struggle with what they have than to be removed (from home).
The HHC nurse experience of safety within a patient’s home was another part of this emergent theme, and was described in the context of caring for patients with behavioral health conditions:
Participant 1: I’m reading the H&P, and it says, you know, he’s got homicidal tendencies and I’m thinking…
Participant 2: Does he have a gun?
Participant 1: …did anybody read this? I mean, what’s going on here? ... and you want me to go there…By myself.
To improve patient safety and health at home, participants described going above and beyond for patients to contribute support beyond clinical care:
We’re there for them. We’re interested in them, and I can’t tell you how many thousands of dollars I’ve probably spent on groceries and medical supplies…that’s a big bugaboo, and that happens across the board...
For facilitating HHC nurse safety, participants emphasized the importance of including key history elements such as cognitive impairment, behavioral health, and psychiatric diagnoses in discharge information available to HHC agencies. Increased information about patient conditions was noted as a key item both for the delivery of appropriate services and for ensuring safety for HHC nurses, who are often alone while visiting patients in their homes.
DISCUSSION
HHC nurses described a range of challenges and solutions to coordinating care for recently discharged patients within the domains of Accountability, Communication, Assessing Needs & Goals, Medication Management, and Safety. Although the focus of group discussions often gravitated to challenges, multiple best practices and aspirations were identified to guide future improvement efforts, as shown in Table 2.
In our study, medication discrepancies were described as a frequent problem in HHC. This aligns with prior studies, in which 94% to 100% of patients had at least one medication discrepancy when HHC and referring provider medication lists were compared.24 , 25 Because adverse events for patients after hospital discharge are most commonly medication-related,26 the high rate of medication discrepancies in HHC may contribute to adverse outcomes for patients. In a Norwegian study exploring HHC nurse perspectives about medication errors in home care, participants identified suboptimal information exchange and communication between clinicians as a contributor to medication errors.10 In another recent study, researchers found that the presence of communication failures between HHC and physicians was associated with a nearly 10% increase in the probability of hospital readmission among high-risk HHC patients with HF.11 Our study illustrates that unclear accountability and inadequate communication likely contribute to medication errors and suboptimal safety for both HHC nurses and patients, which may in turn contribute to adverse patient outcomes such as readmissions.
Solutions discussed by participants could inform multiple quality improvement initiatives to improve care coordination for patients discharged with HHC, as outlined in Table 2. For example, clearly establishing accountability for hospital clinicians in managing HHC orders until PCP follow-up could provide clarity for HHC nurses about whom to contact with questions. Such a solution would address concerns identified by PCPs in our prior qualitative study, who noted challenges in addressing questions from HHC when they had not yet evaluated the patient; PCPs in that study also suggested having hospitalists accountable for HHC for a set amount of time after discharge.17 However, extending hospitalist responsibility for HHC questions would likely require additional social and case management support within the hospital to coordinate and triage HHC requests.
In addition, hospitals and PCPs could improve communication by providing HHC agencies with access to EHRs and direct phone lines. Participants from HHC agencies with read-only access to hospital-based EHRs noted multiple advantages to having this access, including having patient appointment dates and medication lists. Of note, hospitalists and PCPs in our prior study also sought access to direct phone lines and EHRs for clinicians in other clinical settings in order to improve care coordination.17
An example of a policy-level solution that could improve accountability for HHC orders would be giving PAs and NPs the authority to write HHC orders, as proposed in a bill that was recently brought before Congress but was not passed into law (H.R. 1342/S. 3435).27 Broadening HHC order capabilities to PAs and NPs would help facilitate HHC following discharge, particularly in primary care clinics in which an NP may be a patient’s PCP and the clinic may not have a physician, as noted by participants.
In addition to solutions identified in this study, it is important to consider how innovative models of transitional care could be partnered with HHC to address difficulties in care coordination. For example, the Geriatric Resources for Assessment and Care of Elders (GRACE) model includes an NP and social worker assessment in the home for low-income older adults who are eligible for both Medicare and Medicaid.28 The NP and social worker take responsibility for coordinating care for the patient among hospital clinicians, PCPs, HHC clinicians, caregivers, and others during and after hospitalization. This model reduced hospitalization and total health care costs for GRACE participants compared to controls, and could be a promising approach for improving transitional care for other high-risk populations.
Although our focus groups were limited to HHC agencies in the Denver metropolitan area, participants were comparable to workforce estimates of HHC—93% of participants were female, which is comparable to the 89% of the HHC service industry that is female.29 In addition, 83% of HHC agencies in this study were for-profit, which is comparable to the 80% of for-profit HHC agencies nationally.30 Limitations to this work include unknown demographics or perspectives from nurses who may have been invited but opted not to participate in focus groups. Because we limited our study to HHC nurses, we do not have perspectives from other clinicians (e.g., physical therapists) in HHC, which could provide additional context. Our results may not be generalizable beyond the context of study participants.
As the US health system promotes shared accountability for patient outcomes across settings, the need to address fragmentation in care coordination is increasingly important. Our findings in this study suggest that improvements to accountability and communication could address patient needs and goals, avoid medication discrepancies, and ultimately improve safety for patients and HHC nurses. Clinician-led efforts to improve care coordination with HHC should focus on clearly defining physician accountability for HHC orders, improving communication by providing EHR access and direct phone lines for HHC, improving alignment of expectations for HHC between clinicians and patients, coordinating with HHC to reduce medication discrepancies, and prioritizing safety for both patients and HHC nurses by ensuring that cognitive and behavioral health information is provided to HHC clinicians. Future work to better understand HHC patient and caregiver perceptions of care coordination, as well as care needs beyond reimbursable HHC services such as transportation, meal services, and additional caregiving support, could inform efforts to refine reimbursement and inform innovation to support patients’ desires to remain in their homes.31
References
Jones CD, Ginde AA, Burke RE, Wald HL, Masoudi FA, Boxer RS. Increasing Home Healthcare Referrals upon Discharge from U.S. Hospitals: 2001-2012. J Am Geriatr Soc. 2015;63(6):1265–1266.
CMS.gov. Readmissions Reduction Program. 2016; http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. Accessed 21 Dec 2016.
Bundled Payments for Care Improvement (BPCI) Initiative: General Information. 2017; https://innovation.cms.gov/initiatives/bundled-payments/. Accessed 13 Feb 2017.
www.cms.gov. Research Statistics Data and Systems. 2016.
Jones CD, Wald HL, Boxer RS, et al. Characteristics Associated with Home Health Care Referrals at Hospital Discharge: Results from the 2012 National Inpatient Sample. Health Serv Res. 2017;52(2):879–894.
Medicare.gov. Home Health Services. https://www.medicare.gov/coverage/home-health-services.html. Accessed May 31, 2017.
Madigan EA, Gordon NH, Fortinsky RH, Koroukian SM, Pina I, Riggs JS. Rehospitalization in a national population of home health care patients with heart failure. Health Serv Res. 2012;47(6):2316–2338.
Avalere. Medicare Readmission Rates by State: Prepared for the Alliance for Home Health Quality and Innovation. 2016; http://ahhqi.org/images/uploads/20160121_AHHQI_Readmissions_by_State_final_copy.pdf. Accessed 15 Feb 2016.
Hospital Compare. https://www.medicare.gov/hospitalcompare/search.html. Accessed 1 May 2017.
Berland A, Bentsen SB. Medication errors in home care: a qualitative focus group study. J Clin Nurs. 2017.
Pesko MF, Gerber LM, Peng TR, Press MJ. Home Health Care: nurse-physician communication, patient severity, and hospital readmission. Health Serv Res. 2017.
Jones AL, Harris-Kojetin L, Valverde R. Characteristics and use of home health care by men and women aged 65 and over. Natl Health Stat Report. 2012(52):1–7.
Sockolow P, Bass EJ, Eberle CL, Bowles KH. Homecare Nurses' Decision-Making During Admission Care Planning. Stud Health Technol Inform. 2016;225:28–32.
Brega AG, Schlenker RE, Higgazi, K, Neal S, Belansky ES, Talkington S, Jordan AK, Bontrager J, Tennant C. Study of Medicare home health practice variations: final report. Denver, CO. August, 2002.
Centers for Medicare & Medicaid Services. Home Health Patient Tracking Sheet. Baltimore, MD: Centers for Medicare & Medicaid Services; 2009:24.
American Nurses Association. Home Health Nursing: Scope and Standards of Practice. 2nd ed. Silver Spring, MD: American Nurses Association; 2014.
Jones CD, Vu MB, O’Donnell CM, et al. A failure to communicate: a qualitative exploration of care coordination between hospitalists and primary care providers around patient hospitalizations. J Gen Intern Med. 2015;30(4):417–424.
Bowles KH, Pham, J, O’Connor M, Horowitz DA. Information Deficits in Home Care: A Barrier to Evidence-Based Disease Management. Home Health Care Management Practice. 2010;22(4):278–285.
McDonald KM, Sundaram V, Bravata DM, et al. Closing the quality gap: a critical analysis of quality improvement strategies (Vol. 7: Care Coordination). Rockville (MD). 2007.
Thomas DR. A General Inductive Approach for Analyzing Qualitative Evaluation Data. American Journal of Evaluation. 2006;27(2):237–246.
Jones J, Nowels CT, Sudore R, Ahluwalia S, Bekelman DB. The future as a series of transitions: qualitative study of heart failure patients and their informal caregivers. J Gen Intern Med. 2015;30(2):176–182.
Jones J, Nowels C, Kutner JS, Matlock DD. Shared decision making and the use of a patient decision aid in advanced serious illness: provider and patient perspectives. Health Expect. 2015;18(6):3236–3247.
Kerr C, Nixon A, Wild D. Assessing and demonstrating data saturation in qualitative inquiry supporting patient-reported outcomes research. Expert Rev Pharmacoecon Outcomes Res. 2010;10(3):269–281.
Hale J, Neal EB, Myers A, et al. Medication Discrepancies and Associated Risk Factors Identified in Home Health patients. Home Healthc Now. 2015;33(9):493–499.
Brody AA, Gibson B, Tresner-Kirsch D, et al. High Prevalence of Medication Discrepancies Between Home Health Referrals and Centers for Medicare and Medicaid Services Home Health Certification and Plan of Care and Their Potential to Affect Safety of Vulnerable Elderly Adults. J Am Geriatr Soc. 2016;64(11):e166-e170.
Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–167.
S. 578 — 114th Congress: Home Health Care Planning Improvement Act of 2015. 2015.
Bielaszka-DuVernay C. The 'GRACE' model: in-home assessments lead to better care for dual eligibles. Health Aff (Millwood). 2011;30(3):431–434.
Avalere. Home health chartbook 2015: Prepared for the Alliance for Home Health Quality and Innovation. 2016. http://ahhqi.org/images/uploads/AHHQI_2015_Chartbook_FINAL_October_Aug2016Update.pdf. Accessed 15 Dec2016.
Harris-Kojetin L, Sengupta M, Park-Lee E, et al. Long-term care providers and services users in the United States: Data from the National Study of Long-Term Care Providers, 2013-2014. Vital Health Stat 2016; 3:105.
Landers S, Madigan E, Leff B, et al. The Future of Home Health Care: A Strategic Framework for Optimizing Value. Home Health Care Manag Pract. 2016;28(4):262–278.
Author information
Authors and Affiliations
Contributions
The authors would like to acknowledge the valuable contributions of all study participants. The authors also wish to thank Sue Felton for her contributions.
Corresponding author
Ethics declarations
Funders
Dr. Christine D. Jones is supported by grant number K08HS024569 from the Agency for Healthcare Research and Quality for this work. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. This work was supported by a grant from the University of Colorado, School of Medicine, Department of Medicine, Division of General Internal Medicine.
Prior Presentations
This work was presented at the Society of Hospital Medicine meeting in San Diego, California on March 7, 2016 and at the American Geriatrics Society meeting in Long Beach, California, on May 19, 2016.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Electronic supplementary material
ESM 1
(DOCX 12 kb)
Rights and permissions
About this article
Cite this article
Jones, C.D., Jones, J., Richard, A. et al. “Connecting the Dots”: A Qualitative Study of Home Health Nurse Perspectives on Coordinating Care for Recently Discharged Patients. J GEN INTERN MED 32, 1114–1121 (2017). https://doi.org/10.1007/s11606-017-4104-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-017-4104-0