Abstract
Based on spiral 3D tomography a large variety of applications have been developed during the last decade to asses bone mineral density, bone macro and micro structure, and bone strength. Quantitative computed tomography (QCT) using clinical whole body scanners provides separate assessment of trabecular, cortical, and subcortical bone mineral density (BMD) and content (BMC) principally in the spine and hip, although the distal forearm can also be assessed. Further bone macrostructure, for example bone geometry or cortical thickness can be quantified. Special high resolution peripheral CT (hr-pQCT) devices have been introduced to measure bone microstructure for example the trabecular architecture or cortical porosity at the distal forearm or tibia. 3D CT is also the basis for finite element analysis (FEA) to determine bone strength. QCT, hr-pQCT, and FEM are increasingly used in research as well as in clinical trials to complement areal BMD measurements obtained by the standard densitometric technique of dual x-ray absorptiometry (DXA). This review explains technical developments and demonstrates how QCT based techniques advanced our understanding of bone biology.
Similar content being viewed by others
Introduction
Osteoporosis is characterized by low bone mass and microstructural deterioration leading to an increased risk of fracture. Bone mass and, with certain limitations, structure can both be assessed with bone densitometric imaging techniques in vivo. Areal bone mineral density (BMD) as assessed by dual X-ray absorptiometry (DXA) remains the prevailing bone densitometry parameter used in the clinical setting. However, DXA has limitations in its ability to measure the mass distribution in cortical and trabecular bone compartments and in the evaluation of bone geometry and microstructure. This is the domain of quantitative computed tomography (QCT).
Single slice QCT, the foundation of all QCT techniques discussed in this review, was introduced over 3 decades ago [1–3] to assess apparent bone mineral density (BMD) in the trabecular center of the vertebrae and in the distal forearm [4]. Since then, technical advances in clinical CT-technology have led to continuous improvements in QCT applications. In the 1990s, the introduction of spiral CT allowed for 3D acquisition and made possible refined 3D analysis of volumetric data [5]. This in turn extended QCT imaging to the hip. Improved detector technology combined with cone beam acquisition originally developed for μCT opened the door for high resolution peripheral QCT (hr-pQCT) to assess bone architecture in vivo. Finally finite element analysis (FEA), a method developed in mechanical engineering and first applied in an anatomy-specific manner to bone in 1989 [6] is now a mature, validated technique based on 3D CT datasets that integrates BMD with bone geometry and structure to estimate bone strength under various loading conditions [7].
The increasing clinical use and interest in CT-based techniques in the field of osteoporosis is triggered by increasing evidence that measuring not only bone mass and density but also structure and strength are relevant to the estimation of fracture risk and the understanding of potentially differential therapeutic effects. We provide state of the art information on human applications of CT in the field of osteoporosis.
Measuring Mass and Density
QCT is a volumetric technique, (ie, it provides a separate measure of BMD for each voxel of the scanned volume of interest [VOI]). In particular, cortical and the metabolically more active trabecular compartments can be measured separately (Fig. 1). BMD in g/cm3 is calculated from the CT attenuation values by means of a calibration phantom scanned with the patient. The phantom contains different concentrations of hydroxyapatite equivalent material. Bone mineral content (BMC) is the product of BMD and volume. QCT T-scores, analogous to those derived from DXA BMD, can be calculated using appropriate normal reference data but their relevance to clinical care is limited by the considerable discordance from DXA T-scores [8, 9]. DXA T-scores remain the sole basis for the accepted WHO diagnostic criterion for osteoporosis. An adaptation, in which DXA equivalent areal BMD but not true volumetric BMD results are obtained from a 3D QCT dataset (CTXA method; Mindways Inc, Austin, TX) overcomes that limitation of the clinical application of QCT [10]. While many cross-sectional studies have shown the association of QCT with prevalent fracture, so far only a few studies have demonstrated an association between QCT BMD and incident fracture. In the EFFECT study and a similar study conducted in China, both of which included patients with fresh femur fractures [11•, 12], QCT of the hip improved hip fracture discrimination at best marginally when compared with DXA. Similar results were observed in prospective studies of incident hip fracture including the AGES-REYKJAVIK study [13•] and the MrOS studies [14, 15]. In contrast a recent study showed that at the spine, fracture risk prediction was improved by QCT imaging [16••] supporting results from a number of earlier cross-sectional studies [9, 17–20].
QCT of the spine (top) and hip (bottom). Top left: spine segment L1-L3 with intervertebral spaces. Top center: sagittal MPR with periosteal (red) and cortical and subcortical (blue) contours; superior and inferior VOIs are separated. Top right: axial MPR with traditional central elliptical and Siemens Osteo VOIs. Bottom left: analysis VOIs of the proximal femur: head, neck, trochanter, intertrochanter and shaft. Bottom center: bone compartments: cortical (blue), subcortical (yellow) and trabecular (red). Bottom right: oblique cut perpendicular to the neck axis separating the neck into quadrants
Recent innovations for spine and hip QCT analyses were fostered by the interest in better understanding the effects of different pharmacological interventions separately on cortical, subcortical, and trabecular compartments as well in different VOIs, such as the femoral head and neck, trochanter, and intertrochanter in the proximal femur or sub VOIs within the vertebrae [21] (Fig. 1). QCT results have been reported from clinical trials of bisphosphonates [22, 23, 24•, 25–30], PTH [22, 24•, 26–29, 31], raloxifene [32], ronacaleret [24•], denosumab [33], and cathepsin K inhibitors [34]. Almost all of these studies were analyzed by software developed at the University of California (San Francisco, CA), the MIAF software from the University of Erlangen (Erlangen, Germany) or the commercially available and FDA approved QCTPro package (Mindways Inc). In addition to the hip and spine, the radius is also available to evaluation using regular CT equipment [35].
An important aspect in the interpretation of BMD results obtained from QCT is to realize that percentage changes depend on the baseline value. For example an absolute change of 10 mg/cm3 causes a relative change of 10 % in trabecular BMD (assuming an initial value of 100 mg/cm3) but only a 1.25 % increase of cortical BMD (assuming an initial value of 800 mg/cm3). Accordingly, in a recent cross-sectional QCT investigation of age related decreases in BMD a 2- to 5-fold higher percentage loss in trabecular vs cortical bone at all sites in the femur was reported, although absolute losses in trabecular and cortical bone were fairly similar [36]. The physiological, clinical, and biomechanical implications of this discrepancy, ie, the question whether an absolute or percent change is more relevant and for what, remains to be addressed.
Measuring Macrostructure
As QCT is a true 3D imaging modality it can provide structural information beyond BMD and BMC. Of particular renewed interest is the cortex, for example the local measurement of cortical thickness, density, and porosity. With MIAF as well as with the Bone Investigational Toolkit (BIT), an add-on to the QCTPro software, parameters such as integral, trabecular, and cortical cross-sectional areas and cross-sectional moments of inertia as well as endosteal and periosteal circumferences can be measured in slices perpendicular to the femoral neck axis [31, 37, 38]. These parameters can be applied to measures associated with bone strength such as section moduli and buckling ratios.
A principal limitation to accurately assessing the cortex is the limited spatial resolution of clinical CT equipment, of about 0.5 mm. With typical slice thicknesses of 1 mm and in plane pixel sizes of 0.3–0.7 mm the spatial resolution of currently used QCT protocols is usually not isotropic. The limitation in spatial resolution poses a problem in the spine, where the cortex is usually thinner than 0.5 mm as well as for sections of the femoral neck. Various segmentation strategies have been developed but the accuracy of cortical thickness, volume, and BMD measurements remains limited. Based on earlier theoretical results [39, 40] recently a new advanced cortical segmentation method has been proposed for the hip [41•, 42]. Accuracy errors of lower than 5 % for cortical thicknesses down to 0.3–0.4 mm were achieved based on a validation with femoral specimens scanned with hr-pQCT. This new algorithm requires the input of the “true” cortical density, which is measured in the compact bone of the shaft below the lesser trochanter but may differ at the site of the cortical measurement.
Cortical mass and thickness of the hip can now also be elegantly visualized as a topographical map. Using this technique significant cortical thickness reductions in specific anatomical regions and quadrants of the femoral neck and trochanter were identified, corresponding to the areas where the fracture initiated in fractured patients [43]. Using MIAF on QCT hip images, cortical BMD was reported to decrease in the superior quadrants of the neck 2- to 3-fold faster than observed in the inferior quadrants.
While cortical measures are increasingly being reported, trabecular dimensions prevent their accurate structural evaluation from clinical CT scans obtained with commonly used and accepted imaging protocols. Using increased radiation exposure and reducing slice thickness and pixel spacing, a higher resolution in the spine can be achieved. In combination with sophisticated image processing methods this technique (hr-CT) has been applied in vitro to assess fracture risk [44]. In vivo studies were reported in women to evaluate the effects of teriparatide [45] and in men with glucocorticoid-induced osteoporosis [46•, 47]. A comparison with hr-pQCT scans in excised vertebrae using a refined segmentation showed a high correlation of trabecular distance (r 2 = 0.98) [48] although other parameters were not reported. Further validation of hr-CT with μCT data and investigation of the effect of image noise appears crucial to fully understand the limitation of the spatial resolution of CT spine images on the accuracy of segmentation of individual trabeculae.
It is important to note that in in vitro studies often a better image quality is achieved than in vivo studies and therefore results of trabecular structure or texture may not easily be transferable. More work is required to better relate the cortical and trabecular geometric variables discussed in this section to fracture outcomes in untreated and treated patients and to bring these improved techniques to the clinical setting.
Measuring Microstructure
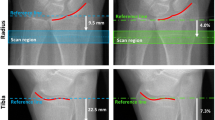
Bone microstructure typically refers to histomorphometric parameters originally obtained from 2D stained sections a few microns thick. This 2D approach has largely been replaced by imaging bone biopsy samples with μCT techniques offering isotropic 3D spatial resolution in the order of 10 μm. This resolution is however not achievable in vivo in humans due to the radiation exposure required. Currently in the distal forearm and tibia a high-resolution peripheral QCT (hr-pQCT) technique has been implemented on the XtremeCT scanner (Scanco, Brütisellen, Switzerland). The scanner provides 3D images with an isotropic voxel size of 41 μm or 82 μm, the latter resulting in isotropic spatial resolution of about 130–150 μm [49•]. With this technique the trabecular architecture can be analyzed resulting in parameters such as BV/TV, Tb.Th, Tb.Sp, and Tb.N in addition to BMD. Also cortical parameters such as BMD, thickness and porosity are calculated [50]. In the field of osteoporosis the technique has been used to predict or discriminate fractures [19, 51–57, 58•], and to assess age [59] and intervention related changes on peripheral bone architecture and BMD [60–68] as well as to investigate bone architecture under various other pathological conditions.
Data on hr-pQCT methods for fracture discrimination are still limited and most publications are based on the Strambo [51, 56] or Ofely studies [52, 55]. For many structural and density hr-pQCT parameters, age adjusted Odds ratios for discriminating fractures were in the range of 1.5–2. However, the contribution of structural parameters of the trabecular compartment became often insignificant after an additional DXA BMD adjustment. In contrast cortical thickness contributed independently of BMD in particular to the discrimination of vertebral fractures [51, 52, 56]. Interestingly, most intervention studies in addition to BMD emphasized hr-pQCT results for cortical thickness and density, and more recently for cortical porosity. In particular, in the radius effects on trabecular architecture parameters often were either not significant [60, 61, 65, 68], added little information to BMD [63] or were difficult to interpret [66].
There are multiple, potentially additive reasons for this observation: first the standard XtremeCT analysis protocol derives BV/TV from the trabecular bone density and an assumed compact bone density of 1200 mg HA/cm3. Therefore BV/TV is highly correlated with trabecular BMD. A fixed, global threshold is used to extract the trabecular structure for direct measurement of trabecular number and then Tb.Th and Tb.Sp are calculated using plate-model assumptions [69, 70]. Thus, changes in mineralization are neglected in the calculation of Tb.Th and Tb.Sp. Advanced segmentation and analysis techniques for the trabecular structure have been researched for hr-pQCT [69, 71–73] but remain largely experimental at present. Of course the underlying problem is the limited spatial resolution, which still causes significant accuracy errors in structural parameters [74•]. Least affected were BV/TV, Tb.N, and Ct.Th, whereas Tb.Th, Ct.Po, and Ct.Po.Dm were affected most. For these variables the correlation between hr-pQCT and μCT measurements, which served as a gold standard, were low or lacked significance.
Another reason is frequent motion artifacts caused by the long scan time of approximately 3 minutes of the devices currently used for the hr-pQCT measurements [75–78]. While more distinct artifacts can be easily recognized and the scan repeated, more subtle motion will cause a blurring of the trabecular network in the reconstructed image and therefore reduce the accuracy of the structural parameters without impacting on BMD results.
Regardless of the limitations, hr-pQCT has already contributed significantly to advance the understanding and interest in bone imaging. This is particularly true for cortical bone. Aging is associated with an increase in total outer bone volume, caused by periosteal apposition, and with cortical thinning and decrease in cortical BMD [79, 80]. The cortical BMD loss is primarily related to an increase in cortical porosity, which cannot be quantified by standard QCT or pQCT imaging due to spatial resolution limits. Cortical porosity increases from the periosteal to the endosteal surface [81] where subendosteal cavitation and conversion of the inner third of the cortex leads to a trabecular like structure [82], also termed trabecularization [83–85] of cortical bone.
Cortical porosity is now a standard parameter of the hr-pQCT analysis [86], however pores much smaller than the spatial resolution of the hr-pQCT scanner may not be properly accounted for due to partial volume artifacts. This is probably one reason why the correlation of cortical porosity results between hr-pQCT and μCT measurements was weak [74•]. This correlation and the accuracy of cortical porosity measurements has been improved by a recent technique that decreases the effect of partial volume artifacts on cortical porosity measurements by specific assumptions on cortical BMD [87•]. The problem of partial volume artifacts will also be much reduced by a separate analysis of the trabecularized part of the cortex where pore size is largely increased. Two recent publications have addressed the importance of such a separate analysis [87•, 88]. The added value of determining porosity over a plain cortical BMD measurement is an area of active research.
Measuring Strength
Strength of a bone can be experimentally determined only in a mechanical test, ie, ex-vivo, where typically the ultimate force necessary to fracture the bone is measured. In vivo we are restricted to an estimation of failure loads using FEA. The complicated problem of calculating deformations and stresses within a bone caused by external loads that may eventually cause fracture is addressed by creating a mesh of elements with known material properties for which equilibrium of forces and moments is enforced at both local and global scales (Fig. 2).
In the bone field, typically μFEA models are distinguished from homogenized FEA models. The former ones require high spatial resolution images so that the elements of the mesh contain bone material only. A segmentation step to separate the individual trabeculae as well as the pores in the compact bone precedes the formation of the mesh model of the bone of interest. Appropriate imaging modalities are μCT, used for specimen work and hr-pQCT [56, 57, 61, 89–94] as well as hr-MRI [95, 96] that can be applied in vivo at the distal forearm and tibia. Dedicated FEA analysis software is available from the manufacturer for the XtremeCT scanner but many research groups use their own proprietary developments.
Thanks to the high resolution of pQCT images available in the past decade, experimental validation of the μFE models progressed to high levels with refined ex vivo biomechanical tests mimicking Colles’ fracture [89, 92, 94, 97]. Interestingly, the outstanding prediction of ultimate load of the distal radius by μFEA was found to be only slightly superior to the one of BMC [98].
While the radius and tibia have enabled important advances in this area, the main fracture sites are the spine and hip, where such a high resolution cannot be achieved. For these skeletal locations homogenized FE models are applied to QCT images obtained from whole body clinical CT-scanners (Fig. 2). A mesh is applied to the entire vertebral body or proximal femur resulting in individual elements with a size in the mm range but higher than the voxel dimensions of the CT dataset containing mineralized bone as well as bone marrow. The term homogenization designates the averaging process to determine the apparent material properties of that mixture of bone and marrow, which are essential input parameters for FEA. Bone is an inhomogeneous, anisotropic and elastic material that undergoes simultaneous plastic deformation and loss of stiffness due to initiation and growth of micro-cracks when overloaded [99, 100].
However, in single energy CT images the only available information of a given voxel is its absorption coefficient or, after proper calibration, its apparent BMD value. The BMD values are linearly or more often non-linearly mapped to the Young’s modulus for bone stiffness and to the yield criterion for failure load [101, 102, 103••, 104–107], which is the main outcome variable. Other parameters such as stress, strain, or damage (loss of stiffness due to microcracks) distribution maps also can be obtained from FEA.
In recent years homogenized FEA of the spine and hip has been applied in epidemiological studies to determine strength or to predict spine [16••, 58•, 108] or hip [109, 110] fractures or to determine changes of bone strength with age [111] or with different treatment [23, 26–28, 34, 112–115]. The accuracy of FEA has been extensively validated using biomechanical tests where the applied forces can be well predicted in the FE model. However, in vivo, the magnitude and direction of external forces, in particular those that occur during a specific fall, can only be estimated [116, 117] and impact the resulting fracture risk prediction. To address this limitation, FEA is often performed on multiple loading conditions such as axial compression, anterior bending, and torsion scenarios in the vertebrae, and for stance and fall scenarios in the proximal femur. Preliminary results indicate that the vertebral body stiffnesses along the different loading scenarios are highly correlated [118]
A performance comparison between FEA and BMD results is difficult. In a recent in vitro study of vertebral sections [119••] FEA was superior to BMD as measured by DXA or QCT but not to BMC in predicting ultimate load. However ultimate load is not size adjusted and larger bones can withstand larger load before they fracture. In the same study, FEA performed only slightly better than BMD as measured by QCT for prediction of the size adjusted parameter apparent ultimate stress. In another in vitro study ultimate load was also better predicted by FEA than by QCT BMD but there BMD was only measured in the trabecular compartment whereas the mechanical tests and the FE calculations were performed on complete vertebral bodies [120]. Femoral strength also was found to be better predicted by FEA than QCT and DXA [121] but in this early study FEA applied to the total proximal femur was compared with QCT and DXA measurements from the neck. In a more recent work, the predictions of femoral strength in stance configuration by FEA were not significantly better than those by BMC measured from QCT [103••].
In MrOs, a cohort study in elderly males, in a retrospective subset analysis ultimate load by FEA in the hip improved fracture prediction, but only marginally compared with DXA [109]. Interestingly in the AGES study male-female differences in the association between incident hip fracture and proximal femoral strength were found [110] although BMD of the hip as measured by DXA predicts hip fractures equally well in both sexes [122]. In MrOs, in the spine, hazard ratios and areas under the curve (AUC) for ultimate load and integral BMD of the total vertebral body were significantly higher than DXA areal BMD [16••]. QCT BMD results were not reported. Similar results in the spine were reported for Japanese women [25], although here no AUC values were given. This is a limitation in particular if reported confidence intervals for hazard or odds ratios from FEA calculations are considerably larger than those for DXA. Even large differences in hazard or odds ratios among techniques may then not be significant. Notwithstanding these limitations there is growing evidence that for fracture prediction at the spine QCT and FEA are superior to DXA.
Several reports on FEA from therapeutic interventions are available. In general the largest treatment-related differences between DXA and FEA results were observed in the spine emphasizing limitations of the projectional DXA technique [23, 26, 34, 47, 112, 113]. Smaller numerical differences were observed at the hip [23, 27, 34, 115] but the significance of the difference was rarely reported. The comparison between FEA and QCT results is even more difficult, in particular, as often QCT and FEA analyses VOIs do not match.
The unique attribute of FEA is the integration of bone geometry and density distribution to calculate bone strength for various load cases. Accordingly FEA can provide additional valuable information. FEA is a rapidly evolving technique and while most FEA software for bone analysis is university based and experimental, one such methodology (ON Diagnostics, Berkley, CA) recently received FDA approval for the use in identification of patients at risk for fracture and follow-up the effect of therapies.
Outlook and Summary
In less than 3 decades since the first report of the QCT methods to measure BMD of the spine and radius, many substantial technical and methodological improvements have been introduced and applied. The CT based techniques reviewed in this article have enabled improved fracture risk prediction, clarification of the pathophysiology of skeletal disease, characterization of the skeletal response to therapy, and enhanced assessment of important biomechanical relationships. They are used extensively in research and increasingly in clinical trials and, over the last decade, have significantly improved our understanding of the organ bone. DXA remains the gold standard in practice, despite its known limitations for monitoring pharmaceutical treatment. However, CT based techniques provide important complementary information. While much remains to be done we can now elegantly visualize and quantitate bone biology in-vivo, thus benefitting science, physician and patient.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Cann CE, Genant HK. Precise measurement of vertebral mineral content using computed tomography. J Comput Assist Tomogr. 1980;4(4):493–500.
Rüegsegger P, Elsasser U, Anliker M, Gnehm H, Kind H, Prader A. Quantification of bone mineralization using computed tomography. Radiology. 1976;121:93–7.
Genant HK, Boyd D. Quantitative bone mineral analysis using dual energy computed tomography. Invest Radiol. 1977;12(6):545–51.
Cann CE. Quantitative CT, for determination of bone mineral density: a review. Radiology. 1988;166:509–22.
Engelke K, Adams JE, Armbrecht G, Augat P, Bogado CE, Bouxsein ML, et al. Clinical use of quantitative computed tomography and peripheral quantitative computed tomography in the management of Osteoporosis in adults: the 2007 ISCD Official Positions. J Clin Densitom. 2008;11(1):123–62.
Faulkner KG, Cann CE, Hasegawa BH. Effect of bone distribution on vertebral strength: assessment with patient-specific nonlinear finite element analysis. Radiology. 1991;179(3):669–74.
Morgan E, Bouxsein M. Use of finite element analysis to assess bone strength. Bonekey Osteovision. 2005;2(12):8–19.
Faulkner KG, von Stetten E, Miller P. Discordance in patient classification using T-scores. J Clin Densitom. 1999;2(3):343–50.
Bergot C, Laval-Jeantet AM, Hutchinson K, Dautraix I, Caulin F, Genant HK. A comparison of spinal quantitative computed tomography with dual energy X-ray absorptiometry in European women with vertebral and nonvertebral fractures. Calcif Tissue Int. 2001;68(2):74–82.
Khoo BC, Brown K, Cann C, Zhu K, Henzell S, Low V, et al. Comparison of QCT-derived and DXA-derived areal bone mineral density and T scores. Osteoporos Int. 2009;20(9):1539–45.
• Bousson VD, Adams J, Engelke K, Aout M, Cohen-Solal M, Bergot C, et al. In vivo discrimination of hip fracture with quantitative computed tomography: results from the prospective European Femur Fracture Study (EFFECT). JBMR. 2011;26(4):881–93. Cross sectional studies comparing QCT and DXA with discriminate fresh femur fractures from controls.
Cheng X, Li J, Lu Y, Keyak J, Lang T. Proximal femoral density and geometry measurements by quantitative computed tomography: association with hip fracture. Bone. 2007;40(1):169–74.
• Johannesdottir F, Poole KE, Reeve J, Siggeirsdottir K, Aspelund T, Mogensen B, et al. Distribution of cortical bone in the femoral neck and hip fracture: a prospective case-control analysis of 143 incident hip fractures; the AGES-REYKJAVIK Study. Bone. 2011;48(6):1268–76. Prospective study with incident hip fractures that specifically investigated hip fracture prediction of various parameters in the neck determined in different neck quadrants. Estimated cortical thickness in the superior-anterior quadrant C best discriminated hip fracture cases from controls.
Black DM, Bouxsein ML, Marshall LM, Cummings SR, Lang TF, Cauley JA, et al. Proximal femoral structure and the prediction of hip fracture in men: a large prospective study using QCT. J Bone Miner Res. 2008;23(8):1326–33.
Yang L, Burton AC, Bradburn M, Nielson CM, Orwoll ES, Eastell R. Distribution of bone density in the proximal femur and its association with hip fracture risk in older men: the MrOS study. J Bone Miner Res. 2012;27(11):2314–24.
•• Wang XA, Sanyal PM, Cawthon L, Palermo M, Jekir J, Christensen KE, et al. Prediction of new clinical vertebral fractures in elderly men using finite element analysis of CT scans. J Bone Miner Res. 2012;27(4):808–16. FEA and QCT show better vertebral fracture predition in men than DXA. Retrospective analysis of the MrOS study.
Duboeuf F, Jergas M, Schott AM, Wu CY, Gluer CC, Genant HK. A comparison of bone densitometry measurements of the central skeleton in post-menopausal women with and without vertebral fracture. Br J Radiol. 1995;68(811):747–53.
Grampp S, Genant HK, Mathur A, Lang P, Jergas M, Takada M, et al. Comparisons of noninvasive bone mineral measurements in assessing age-related loss, fracture discrimination, and diagnostic classification. J Bone Miner Res. 1997;12(5):697–711.
Melton III LJ, Riggs BL, Keaveny TM, Achenbach SJ, Hoffmann PF, Camp JJ, et al. Structural determinants of vertebral fracture risk. J Bone Miner Res. 2007;22(12):1885–92.
Ross PD, Genant HK, Davis JW, Miller PD, Wasnich RD. Predicting vertebral fracture incidence from prevalent fractures and bone density among non-Black, osteoporotic women. Osteoporosis Int. 1993;3(3):120–6.
Engelke K, Fuerst T, Dasic G, Davies RY, Genant HK. Regional distribution of spine and hip QCT BMD responses after one year of once-monthly ibandronate in postmenopausal osteoporosis. Bone. 2010;46(6):1626–32.
Black DM, Bilezikian JP, Ensrud KE, Greenspan SL, Palermo L, Hue T, et al. One year of alendronate after one year of parathyroid hormone (1-84) for osteoporosis. N Engl J Med. 2005;353(6):555–65.
Lewiecki EM, Keaveny TM, Kopperdahl DL, Genant HK, Engelke K, Fuerst T, et al. Once-monthly oral ibandronate improves biomechanical determinants of bone strength in women with postmenopausal osteoporosis. J Clin Endocrinol Metab. 2009;94(1):171–80.
• Fitzpatrick LA, Dabrowski CE, Cicconetti G, Gordon DN, Fuerst T, Engelke K, et al. Ronacaleret, a calcium-sensing receptor antagonist, increases trabecular but not cortical bone in postmenopausal women. J Bone Miner Res. 2012;27(2):255–62. Interesting study comparing effects of 3 different pharmacological treatments (ronacanaleret, alendronate, and teriparatide) on QCT of the spine and hip.
Imai K, Ohnishi I, Matsumoto T, Yamamoto S, Nakamura K. Assessment of vertebral fracture risk and therapeutic effects of alendronate in postmenopausal women using a quantitative computed tomography-based nonlinear finite element method. Osteoporos Int. 2009;20(5):801–10.
Keaveny TM, Donley DW, Hoffmann PF, Mitlak BH, Glass EV, San Martin JA. Effects of teriparatide and alendronate on vertebral strength as assessed by finite element modeling of QCT scans in women with osteoporosis. J Bone Miner Res. 2007;22(1):149–57.
Keaveny TM, Hoffmann PF, Singh M, Palermo L, Bilezikian JP, Greenspan SL, et al. Femoral bone strength and its relation to cortical and trabecular changes after treatment with PTH, alendronate, and their combination as assessed by finite element analysis of quantitative CT scans. J Bone Miner Res. 2008;23(12):1974–82.
Keaveny TM, McClung MR, Wan X, Koppaherdl DL, Mitlak BH, Krohn K. Femoral strength in osteoporotic women treated with teriparatide or alendronate. Bone. 2012;50(1):165–70.
Greenspan SL, Bone HG, Ettinger MP, Hanley DA, Lindsay R, Zanchetta JR, et al. Effect of recombinant human parathyroid hormone (1-84) on vertebral fracture and bone mineral density in postmenopausal women with osteoporosis: a randomized trial. Ann Intern Med. 2007;146(5):326–39.
Eastell R, Lang T, Boonen S, Cummings S, Delmas PD, Cauley JA, et al. Effect of once-yearly zoledronic acid on the spine and hip as measured by quantitative computed tomography: results of the HORIZON Pivotal Fracture Trial. Osteoporos Int. 2010;21(7):1277–85.
Borggrefe J, Graeff C, Nickelsen TN, Marin F, Gluer CC. Quantitative computed tomographic assessment of the effects of 24 months of teriparatide treatment on 3D femoral neck bone distribution, geometry, and bone strength: results from the EUROFORS study. J Bone Miner Res. 2010;25(3):472–81.
Genant HK, Lang T, Fuerst T, Pinette KV, Zhou C, Thiebaud D, et al. Treatment with raloxifene for 2 years increases vertebral bone mineral density as measured by volumetric quantitative computed tomography. Bone. 2004;35(5):1164–8.
McClung MR, Zanchetta JR, Hoiseth A, Kendler DL, Yuen CK, Brown JP, et al. Denosumab densitometric changes assessed by quantitative computed tomography at the spine and hip in postmenopausal women with osteoporosis. J Clin Densitom. 2012;16(2):250–256.
Brixen K, Chapurlat R, Cheung AM, Keaveny TM, Fuerst T, Engelke K, et al. Bone density, turnover, and estimated strength in postmenopausal women treated with odanacatib: a randomized trial. J Clin Endocrinol Metab. 2013;98(2):571–580.
Engelke K, Libanati C, Liu Y, Wang H, Austin M, Fuerst T, et al. Quantitative computed tomography (QCT) of the forearm using general purpose spiral whole-body CT scanners: accuracy, precision and comparison with dual-energy X-ray absorptiometry (DXA). Bone. 2009;45(1):110–8.
Nicks KM, Amin S, Melton LJ III, Atkinson EJ, McCready LK, Riggs BL, et al. Three-dimensional structural analysis of the proximal femur in an age-stratified sample of women. Bone. 2013;55(1):179–188.
Ito M, Nakata T, Nishida A, Uetani M. Age-related changes in bone density, geometry and biomechanical properties of the proximal femur: CT-based 3D hip structure analysis in normal postmenopausal women. Bone. 2011;48(3):627–30.
Bousson V, Le Bras A, Roqueplan F, Kang Y, Mitton D, Kolta S, et al. Volumetric quantitative computed tomography of the proximal femur: relationships linking geometric and densitometric variables to bone strength. Role for compact bone. Osteoporos Int. 2006;17(6):855–64.
Prevrhal S, Fox JC, Shepherd JA, Genant HK. Accuracy of CT-based thickness measurement of thin structures: modeling of limited spatial resolution in all three dimensions. Med Phys. 2003;30(1):1–8.
Prevrhal S, Engelke K, Kalender WA. Accuracy limits for the determination of cortical width and density: the influence of object size and CT imaging parameters. Phys Med Bio. 1999;44:751–64.
• Treece GM, Poole KE, Gee AH. Imaging the femoral cortex: thickness, density and mass from clinical CT. Med Image Anal. 2012;16(5):952–65. Technical paper describing an advanced method for segmenting the cortex in CT images.
Treece GM, Gee AH, Mayhew PM, Poole KE. High resolution cortical bone thickness measurement from clinical CT data. Med Image Anal. 2010;14(3):276–90.
Poole KE, Treece GM, Mayhew PM, Vaculik J, Dungl P, Horak M, et al. Cortical thickness mapping to identify focal osteoporosis in patients with hip fracture. PLoS One. 2012;7(6):e38466.
Ito M, Ikeda K, Nishiguchi M, Shindo H, Uetani M, Hosoi T, et al. Multi-detector row CT imaging of vertebral microstructure for evaluation of fracture risk. J Bone Miner Res. 2005;20(10):1828–36.
Graeff C, Timm W, Nickelsen TN, Farrerons J, Marin F, Barker C, et al. Monitoring teriparatide-associated changes in vertebral microstructure by high-resolution CT in vivo: results from the EUROFORS Study. J Bone Miner Res. 2007;22(9):1426–33.
• Graeff C, Marin F, Petto H, Kayser O, Reisinger A, Pena J, et al. High resolution quantitative computed tomography-based assessment of trabecular microstructure and strength estimates by finite-element analysis of the spine, but not DXA, reflects vertebral fracture status in men with glucocorticoid-induced osteoporosis. Bone. 2013;52(2):568–77. Comparison of QCT, high resolution QCT, FEA, and DXA for association with vertebral deformities in same study.
Gluer CC, Marin F, Ringe JD, Hawkins F, Moricke R, Papaioannu N, et al. Comparative effects of teriparatide and risedronate in glucocorticoid-induced osteoporosis in men: 18-month results of the EuroGIOPs trial. J Bone Miner Res. 2013;28(6):1335–68.
Krebs A, Graeff C, Frieling I, Kurz B, Timm W, Engelke K, et al. High resolution computed tomography of the vertebrae yields accurate information on trabecular distances if processed by 3D fuzzy segmentation approaches. Bone. 2009;44(1):145–52.
• Burghardt AJ, Pialat JB, Kazakia GJ, Boutroy S, Engelke K, Patsch JM, et al. Multi-center precision of cortical and trabecular bone quality measures assessed by HR-PQCT. J Bone Miner Res. 2012;28(3):524–536. Technical study on spatial resolution and phantom precison of nine different hr-pQCT scanners.
Boutroy S, Bouxsein ML, Munoz F, Delmas PD. In vivo assessment of trabecular bone microarchitecture by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab. 2005;90(12):6508–15.
Szulc P, Boutroy S, Vilayphiou N, Chaitou A, Delmas PD, Chapurlat R. Cross-sectional analysis of the association between fragility fractures and bone microarchitecture in older men: the STRAMBO study. J Bone Miner Res. 2011;26(6):1358–67.
Sornay-Rendu E, Cabrera-Bravo JL, Boutroy S, Munoz F, Delmas PD. Severity of vertebral fractures is associated with alterations of cortical architecture in postmenopausal women. J Bone Miner Res. 2009;24(4):737–43.
Vico L, Zouch M, Amirouche A, Frere D, Laroche N, Koller B, et al. High-resolution pQCT analysis at the distal radius and tibia discriminates patients with recent wrist and femoral neck fractures. J Bone Miner Res. 2008;23(11):1741–50.
Stein EM, Liu XS, Nickolas TL, Cohen A, Thomas V, McMahon DJ, et al. Abnormal microarchitecture and reduced stiffness at the radius and tibia in postmenopausal women with fractures. J Bone Miner Res. 2010;25(12):2572–81.
Sornay-Rendu E, Boutroy S, Munoz F, Delmas PD. Alterations of cortical and trabecular architecture are associated with fractures in postmenopausal women, partially independent of decreased BMD measured by DXA: the OFELY study. J Bone Miner Res. 2007;22(3):425–33.
Vilayphiou N, Boutroy S, Szulc P, van Rietbergen B, Munoz F, Delmas PD, et al. Finite element analysis performed on radius and tibia HR-pQCT images and fragility fractures at all sites in men. J Bone Miner Res. 2011;26(5):965–73.
Nishiyama KK, Macdonald HM, Hanley DA, Boyd SK. Women with previous fragility fractures can be classified based on bone microarchitecture and finite element analysis measured with HR-pQCT. Osteoporos Int. 2013;27(5):1733–1740.
• Melton III LJ, Riggs BL, Keaveny TM, Achenbach SJ, Kopperdahl D, Camp JJ, et al. Relation of vertebral deformities to bone density, structure, and strength. J Bone Miner Res. 2010;25(9):1922–30. Comparison of QCT, high resolution pQCT, FEA, and DXA for association with vertebral deformities in same study.
Nicks KM, Amin E, Atkinson J, Riggs BL, Melton III LJ, Khosla S. Relationship of age to bone microstructure independent of areal bone mineral density. J Bone Miner Res. 2012;27(3):637–44.
Chapurlat RD, Laroche M, Thomas T, Rouanet S, Delmas PD, de Vernejoul MC. Effect of oral monthly ibandronate on bone microarchitecture in women with osteopenia-a randomized placebo-controlled trial. Osteoporos Int. 2013;24(1):311–20.
Rizzoli R, Chapurlat RD, Laroche JM, Krieg MA, Thomas T, Frieling I, et al. Effects of strontium ranelate and alendronate on bone microstructure in women with osteoporosis. Results of a 2-year study. Osteoporos Int. 2012;23(1):305–15.
Rizzoli R, Laroche M, Krieg MA, Frieling I, Thomas T, Delmas PD, et al. Strontium ranelate and alendronate have differing effects on distal tibia bone microstructure in women with osteoporosis. Rheumatol Int. 2010;30(10):1341–8.
Macdonald HM, Nishiyama KK, Hanley DA, Boyd DA. Changes in trabecular and cortical bone microarchitecture at peripheral sites associated with 18 months of teriparatide therapy in postmenopausal women with osteoporosis. Osteoporos Int. 2011;22(1):357–62.
Burghardt AJ, Kazakia GJ, Sode M, de Papp AE, Link TM, Majumdar S. A longitudinal HR-pQCT study of alendronate treatment in postmenopausal women with low bone density: relations among density, cortical, and trabecular microarchitecture, biomechanics, and bone turnover. J Bone Miner Res. 2010;25(12):2558–71.
Seeman E, Delmas PD, Hanley DA, Sellmeyer D, Cheung AM, Shane E, et al. Microarchitectural deterioration of cortical and trabecular bone: differing effects of denosumab and alendronate. J Bone Miner Res. 2010;25(8):1886–94.
Belavy DL, Beller G, Ritter Z, Felsenberg D. Bone structure and density via HR-pQCT in 60d bed-rest, 2-years recovery with and without countermeasures. J Musculoskelet Neuronal Interact. 2011;11(3):215–26.
Armbrecht G, Belavy DL, Backstrom M, Beller G, Alexandre C, Rizzoli R, et al. Trabecular and cortical bone density and architecture in women after 60 days of bed rest using high-resolution pQCT: WISE 2005. J Bone Miner Res. 2011;26(10):2399–410.
Lam TP, Ng B.K, Cheung LW, Lee KM, Qin L, Cheng JC. Effect of whole body vibration (WBV) therapy on bone density and bone quality in osteopenic girls with adolescent idiopathic scoliosis: a randomized, controlled trial. Osteoporos Int. 2013;24(5):1623–1636.
Burghardt AJ, Kazakia GJ, Majumdar S. A local adaptive threshold strategy for high resolution peripheral quantitative computed tomography of trabecular bone. Ann Biomed Eng. 2007;35(10):1678–86.
Laib A, Ruegsegger P. Calibration of trabecular bone structure measurements of in vivo three-dimensional peripheral quantitative computed tomography with 28-microm-resolution microcomputed tomography. Bone. 1999;24(1):35–9.
Valentinitsch A, Patsch JM, Burghardt AJ, Link TM, Majumdar S, Fischer L, et al. Computational identification and quantification of trabecular microarchitecture classes by 3-D texture analysis-based clustering. Bone. 2013;54(1):133–40.
Varga P, Zysset PK. Assessment of volume fraction and fabric in the distal radius using HR-pQCT. Bone. 2009;45(5):909–17.
Buie HR, Campbell GM, Klinck RJ, MacNeil JA, Boyd SK. Automatic segmentation of cortical and trabecular compartments based on a dual threshold technique for in vivo micro-CT bone analysis. Bone. 2007;41(4):505–15.
• Tjong W, Kazakia GJ, Burghardt AJ, Majumdar S. The effect of voxel size on high-resolution peripheral computed tomography measurements of trabecular and cortical bone microstructure. Med Phys. 2012;39(4):1893–903. Technical paper providing an overview of the capability of HR-pQCT analysis to accurately measure trabecular and cortical bone parameters. At the standard clinical voxel size of 82 μm, measures of porosity were only moderately correlated to gold standard μCT data suggesting cautious interpretation of HR-pQCT measures of cortical microstructure.
Pialat JB, Burghardt AJ, Sode M, Link TM, Majumdar S. Visual grading of motion induced image degradation in high resolution peripheral computed tomography: impact of image quality on measures of bone density and micro-architecture. Bone. 2012;50(1):111–8.
Pauchard Y, Ayres FJ, Boyd SK. Automated quantification of three-dimensional subject motion to monitor image quality in high-resolution peripheral quantitative computed tomography. Phys Med Biol. 2011;56(20):6523–43.
Sode M, Burghardt AJ, Pialat JB, Link TM, Majumdar S. Quantitative characterization of subject motion in HR-pQCT images of the distal radius and tibia. Bone. 2011;48(6):1291–7.
Engelke K, Stampa B, Timm W, Dardzinski B, de Papp AE, Genant HK, et al. Short-term in vivo precision of BMD and parameters of trabecular architecture at the distal forearm and tibia. Osteoporos Int. 2012;23(8):2151–8.
Khosla S. Pathogenesis of age-related bone loss in humans. J Gerontol A Biol Sci Med Sci. 2012.
Riggs BL, Melton III LJ, Robb RA, Camp JJ, Atkinson EJ, Peterson JM, et al. Population-based study of age and sex differences in bone volumetric density, size, geometry, and structure at different skeletal sites. J Bone Miner Res. 2004;19(12):1945–54.
Bousson V, Bergot C, Meunier A, Barbot F, Parlier-Cuau C, Laval-Jeantet AM, et al. CT of the middiaphyseal femur: cortical bone mineral density and relation to porosity. Radiology. 2000;217(1):179–87.
Parfitt AM. Age-related structural changes in trabecular and cortical bone: cellular mechanisms and biochemical consequences. Calcif Tissue Int. 1984;36:S123–8.
Simmons Jr ED, Pritzker KP, Grynpas MD. Age-related changes in the human femoral cortex. J Orthop Res. 1991;9(2):155–67.
Bell KL, Loveridge N, Jordan GR, Power J, Constant CR, Reeve J. A novel mechanism for induction of increased cortical porosity in cases of intracapsular hip fracture. Bone. 2000;27(2):297–304.
Bell KL, Loveridge N, Power J, Garrahan N, Meggitt BF, Reeve J. Regional differences in cortical porosity in the fractured femoral neck. Bone. 1999;24(1):57–64.
Burghardt AJ, Buie HR, Laib A, Majumdar S, Boyd SK. Reproducibility of direct quantitative measures of cortical bone microarchitecture of the distal radius and tibia by HR-pQCT. Bone. 2010;47(3):519–28.
• Zebaze R, Zadeh AG, Mbala A, Seeman E. A new method of segmentation of compact-appearing, transitional and trabecular compartments and quantification of cortical porosity from high resolution peripheral quantitative computed tomographic images. Bone. 2013;54(1):8–20. Technical paper describing the segmentation and analysis of a transitional or cortico-trabecular junctional zone in hr-pQCT images.
Zebaze RM, Ghasem-Zadeh A, Bohte A, Iuliano-Burns S, Mirams M, Price RI, et al. Intracortical remodelling and porosity in the distal radius and post-mortem femurs of women: a cross-sectional study. Lancet. 2010;375(9727):1729–36.
Mueller TL, Christen D, Sandercott S, Boyd SK, van Rietbergen B, Eckstein F, et al. Computational finite element bone mechanics accurately predicts mechanical competence in the human radius of an elderly population. Bone. 2011;48(6):1232–8.
Dalzell N, Kaptoge S, Morris N, Berthier A, Koller B, Braak L, et al. Bone micro-architecture and determinants of strength in the radius and tibia: age-related changes in a population-based study of normal adults measured with high-resolution pQCT. Osteoporos Int. 2009;20(10):1683–94.
Boutroy S, Van Rietbergen B, Sornay-Rendu E, Munoz F, Bouxsein ML, Delmas PD. Finite element analysis based on in vivo HR-pQCT images of the distal radius is associated with wrist fracture in postmenopausal women. J Bone Miner Res. 2008;23(3):392–9.
Pistoia W, van Rietbergen B, Lochmuller EM, Lill CA, Eckstein F, Ruegsegger P. Image-based micro-finite-element modeling for improved distal radius strength diagnosis: moving from bench to bedside. J Clin Densitom. 2004;7(2):153–60.
Jayakar RY, Cabal A, Szumiloski J, Sardesai S, Phillips EA, Laib A, et al. Evaluation of high-resolution peripheral quantitative computed tomography, finite element analysis and biomechanical testing in a pre-clinical model of osteoporosis: a study with odanacatib treatment in the ovariectomized adult rhesus monkey. Bone. 2012;50(6):1379–88.
Varga P, Baumbach S, Pahr D, Zysset PK. Validation of an anatomy specific finite element model of Colles' fracture. J Biomech. 2009;42(11):1726–31.
Newitt DC, van Rietbergen B, Majumdar S. Processing and analysis of in vivo high-resolution MR images of trabecular bone for longitudinal studies: reproducibility of structural measures and micro-finite element analysis derived mechanical properties. Osteoporos Int. 2002;13(4):278–87.
Newitt DC, Majumdar S, van Rietbergen B, von Ingersleben G, Harris ST, Genant HK, et al. In vivo assessment of architecture and micro-finite element analysis derived indices of mechanical properties of trabecular bone in the radius. Osteoporos Int. 2002;13(1):6–17.
MacNeil JA, Boyd SK. Bone strength at the distal radius can be estimated from high-resolution peripheral quantitative computed tomography and the finite element method. Bone. 2008;42(6):1203–13.
Varga P, Pahr DH, Baumbach S, Zysset PK. HR-pQCT based FE analysis of the most distal radius section provides an improved prediction of Colles' fracture load in vitro. Bone. 2010;47(5):982–8.
Zysset PK, Curnier A. A 3D damage model for trabecular bone based on fabric tensors. J Biomech. 1996;29(12):1549–58.
Nalla RK, Kinney JH, Ritchie RO. Mechanistic fracture criteria for the failure of human cortical bone. Nat Mater. 2003;2(3):164–8.
Keyak JH, Lee IY, Skinner HB. Correlations between orthogonal mechanical properties and density of trabecular bone: use of different densitometric measures. J Biomed Mater Res. 1994;28(11):1329–36.
Keller TS. Predicting the compressive mechanical behavior of bone. J Biomech. 1994;27(9):1159–68.
•• Dall'Ara E, Luisier B, Schmidt R, Kainberger F, Zysset P, Pahr D. A nonlinear QCT-based finite element model validation study for the human femur tested in two configurations in vitro. Bone. 2013;52(1):27–38. Elaborate in vitro study to compare correlations of QCT BMD and BMC and FEA with ultimate force and stiffness in stance and lateral loading conditions.
Keyak JH, Falkinstein Y. Comparison of in situ and in vitro CT scan-based finite element model predictions of proximal femoral fracture load. Med Eng Phys. 2003;25(9):781–7.
Bayraktar HH, Morgan EF, Niebur GL, Morris GE, Wong EK, Keaveny TM. Comparison of the elastic and yield properties of human femoral trabecular and cortical bone tissue. J Biomech. 2004;37(1):27–35.
Kopperdahl DL, Morgan EF, Keaveny TM. Quantitative computed tomography estimates of the mechanical properties of human vertebral trabecular bone. J Orthop Res. 2002;20(4):801–5.
Helgason B, Perilli E, Schileo E, Taddei F, Brynjolfsson S, Viceconti M. Mathematical relationships between bone density and mechanical properties: a literature review. Clin Biomech. 2008;23(2):135–46.
Amin S, Kopperdhal DL, Melton III LJ, Achenbach SJ, Therneau TM, Riggs BL, et al. Association of hip strength estimates by finite-element analysis with fractures in women and men. J Bone Miner Res. 2011;26(7):1593–600.
Orwoll ES, Marshall LM, Nielson CM, Cummings SR, Lapidus J, Cauley JA, et al. Finite element analysis of the proximal femur and hip fracture risk in older men. J Bone Miner Res. 2009;24(3):475–83.
Keyak JH, Sigurdsson S, Karlsdottir G, Oskarsdottir D, Sigmarsdottir A, Zhao S, et al. Male-female differences in the association between incident hip fracture and proximal femoral strength: a finite element analysis study. Bone. 2011;48(6):1239–45.
Keaveny TM, Kopperdahl DL, Melton III LJ, Hoffmann PF, Amin S, Riggs BL, et al. Age-dependence of femoral strength in white women and men. J Bone Miner Res. 2010;25(5):994–1001.
Mawatari T, Miura H, Hamai S, Shuto T, Nakashima Y, Okazaki K, et al. Vertebral strength changes in rheumatoid arthritis patients treated with alendronate, as assessed by finite element analysis of clinical computed tomography scans: a prospective randomized clinical trial. Arthritis Rheum. 2008;58(11):3340–9.
Graeff C, Chevalier Y, Charlebois M, Varga P, Pahr D, Nickelsen TN, et al. Improvements in vertebral body strength under teriparatide treatment assessed in vivo by finite element analysis: results from the EUROFORS study. J Bone Miner Res. 2009;24(10):1672–80.
Chevalier Y, Quek E, Borah B, Gross G, Stewart J, Lang T, et al. Biomechanical effects of teriparatide in women with osteoporosis treated previously with alendronate and risedronate: results from quantitative computed tomography-based finite element analysis of the vertebral body. Bone. 2010;46(1):41–8.
Lian KC, Lang TF, Keyak JH, Modin GW, Rehman Q, Do L, et al. Differences in hip quantitative computed tomography (QCT) measurements of bone mineral density and bone strength between glucocorticoid-treated and glucocorticoid-naive postmenopausal women. Osteoporos Int. 2005;16(6):642–50.
Buckley JM, Kuo CC, Cheng LC, Loo K, Motherway J, Slyfield C, et al. Relative strength of thoracic vertebrae in axial compression vs flexion. Spine J. 2009;9(6):478–85.
Bessho M, Ohnishi I, Matsumoto T, Ohashi S, Matsuyama J, Tobita K, et al. Prediction of proximal femur strength using a CT-based nonlinear finite element method: differences in predicted fracture load and site with changing load and boundary conditions. Bone. 2009;45(2):226–31.
Chevalier Y, Zysset PK. A patient-specific computer tomography-based finite element methodology to calculate the six dimensional stiffness matrix of human vertebral bodies. J Biomech Eng. 2012;134(5):051006.
•• Dall'Ara E, Pahr D, Varga P, Kainberger F, Zysset P. QCT-based finite element models predict human vertebral strength in vitro significantly better than simulated DEXA. Osteoporos Int. 2012;23(2):563–72. Comparison of BMC, BMD as measured by QCT, and DXA as well as of FEA estimates with bone strength related material (ultimate strength and Young's modulus) and structure properties (ultimate force and stiffness).
Crawford RP, Cann CE, Keaveny TM. Finite element models predict in vitro vertebral body compressive strength better than quantitative computed tomography. Bone. 2003;33(4):744–50.
Cody DD, Gross GJ, Hou FJ, Spencer HJ, Goldstein SA, Fyhrie DP. Femoral strength is better predicted by finite element models than QCT and DXA. J Biomech. 1999;32(10):1013–20.
Johnell O, Kanis JA, Oden A, Johansson H, De Laet C, Delmas P, et al. Predictive value of BMD for hip and other fractures. J Bone Miner Res. 2005;20(7):1185–94.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
K Engelke is a part time employee of Synarc and has served on SABs for Amgen, Merck and Ono. T. Fuerst an employee of Synarc and has served on SABs for Merck and Ono. C Libanati is an employee of Amgen. P Zysset has institutional grants from Lilly and Amgen and has received a speaker honorarium from Lilly and Amgen. HK Genant has served on SABs for ONO, Merck, Amgen, Lilly, Pfizer, Janssen, Novartis and Servier.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Engelke, K., Libanati, C., Fuerst, T. et al. Advanced CT based In Vivo Methods for the Assessment of Bone Density, Structure, and Strength. Curr Osteoporos Rep 11, 246–255 (2013). https://doi.org/10.1007/s11914-013-0147-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-013-0147-2