Abstract
Introduction
Postoperative acute kidney injury (AKI) following arthroplasty has not been well studied. Our aim was to identify factors associated with increased risk of AKI.
Methods
The medical records for adult patients who underwent elective total joint arthroplasty during June 1, 2007 to May 31, 2010 at the Mayo Clinic were reviewed to identify patients with normal preoperative kidney function who experienced perioperative AKI, defined as an increase in serum creatinine (sCr) by 26.4 μmol·L−1. For each AKI case, two controls were identified and matched for age, sex, and type of operation. Medical records were abstracted for demographics, comorbid conditions, and preoperative, intraoperative, and postoperative variables. Conditional logistic regression analyses were performed to identify risk factors for AKI.
Results
Of the 9,171 patients who underwent joint replacement operations, 167 with normal preoperative renal function developed AKI with a median [25th, 75th] increase in sCr of 35.4 [26.4, 44.2] μmol·L−1. No patient required dialysis. A higher than normal body mass index, diabetes mellitus, the number of baseline antihypertensive medications, cerebral or peripheral vascular disease, use of general anesthesia, and perioperative blood transfusions were independently associated with risk for AKI. Hospital length of stay and intensive care admissions were greater in AKI patients, and in 12.0% of patients, sCr remained at least 26.4 μmol·L−1 higher than preoperative baseline at least three months after surgery.
Conclusion
In this case-control investigation, we identified several factors associated with the development of postoperative AKI. Recognition of these risk factors could allow for the adoption of perioperative renal protective strategies in patients undergoing arthroplasty.
Résumé
Introduction
La lésion rénale aiguë (LRA) postopératoire après arthroplastie n’a pas été bien étudiée. Notre objectif était d’identifier des facteurs associés à une élévation du risque de LRA.
Méthodes
Les dossiers médicaux de patients adultes ayant subi une arthroplastie totale programmée entre le 1er juin 2007 et le 31 mai 2010 à la Mayo Clinic ont été passés en revue pour identifier les patients ayant une fonction rénale normale avant l’intervention et ayant présenté une LRA périopératoire, définie par une augmentation de la créatinine sérique de 26.4 μmol·L−1. Deux cas témoins appariés pour l’âge, le sexe et le type d’intervention ont été identifiés pour chaque cas de LRA. Des dossiers médicaux, on a retenu les données démographiques, les comorbidités et les variables pré- per- et postopératoires. Des analyses de régression logistique conditionnelle ont été réalisées pour identifier les facteurs de risque de LRA.
Résultats
9 171 patients ont subi des interventions de remplacement articulaire et, parmi eux, 167 patients qui avaient une fonction rénale préopératoire normale ont développé une LRA avec une augmentation moyenne (25e, 75e) de la créatinine de 35.4 (26.4, 44.2) μmol·L−1. Aucun patient n’a nécessité de dialyse. Les facteurs associés de façon indépendante au risque de LRA étaient un indice de masse corporelle élevé; le diabète; le nombre de médicaments antihypertenseurs à l’inclusion; une maladie vasculaire cérébrale ou périphérique; le recours à l’anesthésie générale; et les transfusions de sang en période périopératoire. La durée de l’hospitalisation et les admissions aux soins intensifs ont été plus importants parmi les patients atteints de LRA et la créatinine est restée supérieure à 26.4 μmol·L−1 plus de trois mois après la chirurgie chez 12 % des patients, par rapport à la valeur à l’inclusion.
Conclusion
Dans cette étude cas-témoins, nous avons identifié plusieurs facteurs associés à l’apparition d’une LRA postopératoire. L’identification de ces facteurs de risque pourrait permettre l’adoption de stratégies de protection rénale chez les patients subissant une arthroplastie.
Similar content being viewed by others
Total joint arthroplasty is a frequently performed operation and demand is likely to increase.1,2 The occurrence of complications, such as stroke and myocardial infarctions, is estimated to be 0.2% and 1.5%, respectively;3,4 however, little is known about patients undergoing total joint arthroplasty who develop acute kidney injury (AKI). Postoperative AKI is a serious complication, and identification of any modifiable factors could assist in perioperative management. At present, most studies that have tried to define these factors have examined heterogenous surgical populations.5 In contrast, AKI following joint arthroplasty has not been well characterized, and to date, few studies on this topic have been published.6,7 The primary aim of the present study is to undertake further exploration of the preoperative and intraoperative factors associated with postoperative AKI in patients undergoing total joint arthroplasty.
Methods
This study was approved by the Mayo Clinic, Rochester MN, Institutional Review Board. Consistent with Minnesota Statute 144.335 Subd. 3a. (d), we included only patients who have provided authorization for research use of their medical records.Footnote 1 To assess for factors associated with postoperative AKI, we utilized a retrospective 2:1 matched case-control study design. For each case, a pool of ten potential controls were matched for sex, age (standard deviation, 5 yr), and type of orthopedic procedure. From each pool, two matches were randomly selected. The 2:1 matching design was selected after weighing statistical considerations along with the resources required to abstract medical records. Also, the matching criteria limited the availability of eligible controls for additional matches.
To identify adult patients who underwent elective hip, knee, or shoulder arthroplasty during June 1, 2007 to May 31, 2010, we utilized the Mayo Clinic Total Joint Registry Database.8 This computerized database is designed to determine the effectiveness of arthroplasty surgery as a function of implant design, surgical technique, and patient selection, and the database includes all patients receiving joint replacement at the Mayo Clinic (Rochester, MN, USA). It has been maintained for over 40 years and has been used for numerous orthopedic surgery outcomes studies.8 The study timeframe of a three-year epoch was selected based on two assumptions: 1) it would be adequate to identify a sufficient number of AKI cases (> 100) to perform a meaningful analysis; and 2) it would minimize the effects of practice change over time. Only the first surgery was considered for those patients who had multiple procedures during the study timeframe. Exclusion criteria included patients who required an emergent operation or surgery involving infection, trauma, or pathologic fracture repair. The Mayo Clinic and International Business Machines (IBM) Corporation have collaboratively developed a sophisticated data warehouse (Mayo Clinic Life Sciences System [MCLSS]), which contains a replicate of Mayo Clinic’s electronic medical record.9 The MCLSS is developed from multiple clinical data sources, including full-text clinical notes, laboratory tests, diagnostic findings, demographics, and related clinical data. The electronic medical record data are loaded into MCLSS using IBM’s WebSphere Commerce Analyzer, creating DB/2 Universal Database structures of Mayo Clinic’s normalized clinical data. The MCLSS provides a query-building tool, Data Discovery and Query Builder (DDQB). For this study, the DDQB was used to extract serum creatinine (sCr) concentrations obtained within six months antecedent to surgery (baseline value) and within the first 72 hr postoperatively. This timeframe was selected to limit analysis of causative factors to the immediate postoperative period. Patients without baseline and postoperative sCr were excluded. Only patients with normal preoperative renal function—as defined by a glomerular filtration rate ≥ 60 mL·min−1/1.73 m−2 (calculated using the Modification of Diet in Renal Disease Study equation)10—were included.
Assessment of AKI
A comparison between baseline and highest postoperative sCr was performed to determine the presence of postoperative AKI. Typically, preoperative sCr is measured during the preanesthetic evaluation, and postoperative sCr is measured by the surgical service on postoperative day one or two; however, there is no standing protocol for measurement of preoperative and postoperative sCr. The development of AKI was defined using a modification of the Acute Kidney Injury Network (AKIN) criteria. The AKIN criteria is a minimal increase of sCr by 26.4 μmol·L−1 within a 48-hr period.11 We used sCr obtained within the first 48 postoperative hours to determine the presence or absence of AKI; however, when no postoperative sCr was obtained during that initial period, we used the value obtained within 49-72 postoperative hours. This AKIN criteria modification has the potential for misclassifying some patients as having AKI when the increase in sCr was < 26.4 μmol·L−1 in the first 48 hr but was unmeasured until the third postoperative day. Decline in urine output was not used because of inaccuracies of such measurements on postoperative wards. The severity of AKI was characterized using the AKIN staging system11 into three grades: Stage 1 = sCr increase ≥ 26.4 μmol·L−1 or increase ≥ 150-200% from baseline value; Stage 2 = sCr increase ≥ 200%; Stage 3 = sCr increase ≥ 300% or need for dialysis.
Anesthetic management
The anesthetic for patients undergoing arthroplasty generally consists of peripheral nerve blocks (i.e., femoral nerve block) and neuraxial or general anesthetic, at the anesthesiologist’s discretion. Part of the perioperative analgesic regimen relied on nonsteroidal anti-inflammatory drugs (NSAID), celecoxib 200-400 mg orally preoperatively or ketorolac 15-30 mg perioperatively, as deemed appropriate by the attending anesthesiologist.
Data abstraction
All data were abstracted from the electronic medical records and entered manually into the web-based Research Electronic Data Capture (REDCap®) system version 3.6.7 (Vanderbilt University, Nashville, TN, USA).12 All data were abstracted by one anesthesia research fellow (C.G.) and four student nurse anesthetists (P.D.J., D.R.B., N.J.B., R.D.C.). To achieve the uniformity of data extraction, the first ten charts were reviewed by all abstractors and differences were reconciled in a discussion with the two senior authors (T.N.W., J.S.). Electronic medical records were abstracted for demographics, comorbid conditions, and preoperative, intraoperative and postoperative variables. Comorbid conditions were defined according to definitions used for numerous outcome studies at Mayo Clinic,13 including cardiac disease, coronary artery disease (myocardial infarction, coronary stent placement, or cardiac bypass surgery), congestive heart failure/cardiomyopathy (or ejection fraction < 40%), cardiac dysrhythmia (atrial fibrillation or flutter, implanted pacemaker, and/or automated defibrillator), arterial hypertension (medically treated), cerebral or peripheral vascular disease, diabetes mellitus (medically treated), hyperlipidemia (medically treated), and anemia (WHO criteria of anemia).14 The number of antihypertensive medications used by hypertensive patients was recorded. Overall physical status was assessed from the American Society of Anesthesiologists’ physical status score.
The anesthetic record was reviewed for anesthetic duration, anesthetic method (neuraxial vs general anesthesia), blood transfusion, and perioperative complications, including severe hemodynamic instability (need for vasopressor medications beyond ephedrine or phenylephrine, cardiopulmonary resuscitation, or other advanced resuscitative techniques) or other severe perioperative complications.
Postoperative complications and mortality that occurred within 30 postoperative days were reported, and the status of kidney function at three months or later after surgery was documented.
Data analysis
Potential comorbid conditions that could be associated with AKI as well as type and duration of anesthesia and perioperative blood transfusions were assessed using conditional logistic regression taking into account the 1:2 matched set study design. In addition to univariable regression analyses, a multivariable logistic regression analysis was performed with all characteristics listed in Table 1 included as explanatory variables. Explanatory variables were selected based on a systematic review of the literature. This search was conducted using Ovid MEDLINE® and Embase search engines from 2000-2010 using the following search terms: “kidney injury”; “kidney failure”; “arthroplasty, replacement, hip”; “hip prosthesis”; “joint prosthesis”; “knee prosthesis”; and “arthroplasty, replacement, knee”. Retrieved manuscripts were manually reviewed to identify studies that specifically studied postoperative kidney injury following elective total joint arthroplasty surgery. This search identified two studies.6,7 Two large published studies that examined AKI following general surgery using the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) were also used to identify potential explanatory variables.15,16 Generally, age, sex, preexisting renal disease, components of the metabolic syndrome, cardiovascular disease, and surgical complexity have been evaluated.6,7,15,16 As age and sex were matching criteria and preexisting kidney disease an exclusion criteria, these variables were not examined in this study. Findings from the logistic regression analyses are summarized by presenting the odds ratios and corresponding 95% confidence intervals. Two-tailed P values ≤ 0.05 were considered statistically significant. Analyses were performed using SAS® statistical software version 9.2 (SAS Institute, Inc., Cary, NC, USA).
Results
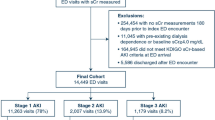
During the study period, 9,171 patients underwent one or more joint replacement surgeries (only index procedures were considered for analysis). Preoperative sCr was obtained for 8,095 patients and postoperative sCr for 8,220 patients. Both preoperative and postoperative sCr concentrations were obtained in 7,463 patients. We identified 167 patients with normal preoperative renal function who experienced a postoperative increase in sCr consistent with AKI. The median [25th, 75th] increase in sCr was 35.4 [26.4, 44.2] μmol·L−1. All but 11 episodes were AKIN Stage I injuries. All cases were matched 2:1 with control patients, and by study design, both groups were of similar age, same sex, underwent identical types of surgery, and had a normal preoperative glomerular filtration rate (GFR) (Table 1). Table 2 summarizes specific comorbidities and surgical characteristics associated with the development of postoperative AKI. A secondary analysis restricted to known preoperative variables yielded similar odds ratio estimates, although the finding was no longer significant for diabetes mellitus. Table 3 summarizes the intraoperative and postoperative course of cases and controls. Serum creatinine concentrations obtained at least three months following surgery were available for 83 (49.7%) cases and 252 (75.4%) controls, and 12.0% of cases continued to have sCr elevated (≥ 26.4 μmol·L−1) from preoperative baseline levels. In comparison, 1.7% of controls were found to have elevated sCr from preoperative baseline levels after three months.
Discussion
In orthopedic patients with normal preoperative kidney function, higher than normal body mass index (BMI), diabetes mellitus, hypertension, cerebrovascular or peripheral vascular disease, exposure to general anesthesia, and blood transfusions were independent risks for development of postoperative AKI. These findings suggest that chronic diseases known to lead to the development of chronic kidney disease17 also play a role in perioperative AKI. Although the majority of injuries were Stage I, any increase in sCr reflects a clinically relevant decrement in GFR, which may be associated with long-term risk of impaired renal function.18 Indeed, 12% of patients did not have normalization of kidney function.
Studies of postoperative kidney injury have suffered from a lack of consistency in defining AKI.19 The RIFLE criteria19 and subsequent AKIN definition11 have addressed this methodological deficiency. Acute kidney injury following cardiac, vascular surgery, and major noncardiac surgery has been well studied;5,16,20-23 however, AKI following joint arthroplasty has received less attention.6,7,24 Though our study was not designed to determine the incidence of postoperative AKI, the percentage of cases (1.8%) that experienced postoperative AKI is higher than previous estimates (0.4-0.55%), likely reflecting increased sensitivity of our modified AKIN criteria compared with RIFLE criteria,11,19 which may introduce an ascertainment bias.
Two studies have examined factors associated with AKI following joint arthroplasty.6,7 Jafari et al.6 reported that increased BMI, preoperative sCr, surgical duration, chronic obstructive pulmonary disease, liver disease, hypertension, and heart disease were independent risk factors for postoperative AKI. Aveline et al.7 found that preoperative kidney dysfunction, advanced age, comorbidities, and prolonged use of NSAIDS were associated with postoperative renal dysfunction. The current study differed in that patients with pre-existing kidney disease were excluded and matched for age, and a more detailed analysis of perioperative management was performed. Similar to Jafari et al.,6 we found that a higher than normal BMI represents an increased risk for AKI. A large study of over 300,000 patients undergoing noncardiac surgery from the ACS-NSQIP database found that the risk of postoperative AKI was increased by three- to seven-fold in obese compared with normal-weight patients.15 Obesity is linked to metabolic syndrome,25 a condition associated with chronic kidney disease.17 While the presence of metabolic syndrome was not assessed directly, it is plausible that syndrome components (diabetes, hypertension, hyperlipidemia, glucose intolerance, or insulin resistance) may have acted in concert to increase risk, though parsing the relevance of individual factors is challenging. Data from the ACS-NSQIP found that diabetics were 1.3 (for those on oral therapy) to 1.7 (for those on insulin therapy) times more likely to develop postoperative AKI,16 a degree of increased risk comparable with our findings. Insulin resistance results in widespread endothelial dysfunction and impaired renal vascular autoregulation26 and has been shown in murine models to worsen kidney injury following ischemia.27 Arterial hypertension has been associated with postoperative AKI in noncardiac16,23 and orthopedic surgical patients.6 In our study, this association was increased with the number of used antihypertensive medications, which provides a clinically relevant means to assess for the risk of postoperative kidney injury. Multiple antihypertensive medications may denote less-controllable hypertension, which could render kidneys more prone to injury.28 Alternatively, multiple antihypertensives could have resulted in intraoperative renal hypoperfusion and subsequent AKI. A post-hoc analysis found no antihypertensive medication class effect. Unfortunately, we do not have information whether our patients took antihypertensive medications the day before or on the day of surgery. The lack of this information precludes us from making a conclusion regarding the role of antihypertensives and the risk of AKI, and this question needs further study.
Arthroplasty performed under general anesthesia was associated with higher AKI risk than those performed under only neuraxial blocks. Epidural analgesia has been shown to have a renal protective effect in patients undergoing coronary artery bypass grafting surgery.29 Though neuraxial anesthesia has little effect on renal blood flow or urine output,30 it does blunt the sympathetic response to surgery, and this has been postulated to be the mechanism of renal protection in open heart surgery.29 Our study design was not designed to elicit the “protective” effect of this technique. It should be emphasized that most patients had peripheral nerve blocks regardless of the primary anesthetic. These peripheral blocks may have also blunted the sympathetic response to surgical incision. In addition, our observation may reflect selection bias towards the favourable use of neuraxial anesthesia in more straightforward (non-complicated or lower-risk) cases.
Perioperative blood transfusions were associated with increased risk of AKI. It is not clear whether this effect can be attributed to anemia, hypovolemia, or to transfusion of blood products per se. However, our model found blood transfusions, but not preoperative anemia, to be independently associated with increased risk. Blood transfusions have increasingly been implicated with postoperative morbidity and mortality, and blood transfusions in septic patients were associated with increased rates of AKI.31 Anemic patients undergoing cardiac surgery who received blood transfusions are at increased risk for AKI;32-34 however, whether reduction of the rate of blood transfusion lowers the incidence of AKI following orthopedic surgery requires further study.35
The rate of perioperative NSAID administration was greater among our controls than the cases. This study was not designed to examine the association between ketorolac administration and kidney injury. The lower rate among cases may reflect selection bias not to administer these medications to those deemed at higher risk for AKI. These medications affect renal autoregulation via impaired synthesis of renal prostaglandins, which reduces renal plasma flow and GFR.36,37 In surgical patients with normal renal function, a transient decrement in renal function is observed but considered to be clinically irrelevant,38 but in the setting of stressed kidneys, continued NSAID administration should be avoided.36,39 Nevertheless, it is unknown if withholding NSAIDS from patients at higher risk of injury would affect the rate or magnitude of AKI.
Outcomes of patients with AKI
It is unclear if the higher rates of ICU admission or longer hospital stays were a result of AKI or other factors (more complicated surgery or patients with greater disease burden who required increased levels of postoperative care). In a minority of AKI patients, renal function did not return to preoperative levels three months after surgery, raising the possibility that injury in some individuals may have a long-term deleterious effect. The risk of eventual development of chronic kidney disease following an episode of postoperative Stage I AKIN is not known; however, it has been suggested that patients who survive an episode of AKI are at greater risk of later developing chronic kidney disease.40
Limitations
This study suffers from limitations inherent in retrospective studies. Since 19% of patients did not have sCr measurements, the observed rate may reflect an underestimate. Our timeframe for sCr was 72 postoperative hours in order to focus our analysis on preoperative and immediate perioperative factors associated with AKI. This may have resulted in missing some AKI cases because sCr may have a delayed rise in response to renal insult. A sizable proportion of our patients, especially those who developed AKI, did not have sCr measurements taken after three months, which impairs our ability to assess long-term outcomes. Our findings reflect an experience in a large tertiary care institution with a relatively homogenous surgical population (almost exclusively white), which limits the generalizability to other populations or practices. Another factor that might reduce the generalizability is the fact that we excluded patients with pre-existing chronic kidney disease and those who underwent emergent surgery or surgery for pathological fractures or infections. These conditions may increase the risk of postoperative AKI.
In conclusion, the rate of postoperative AKI following major elective orthopedic arthroplasty is approximately 2%, most of which was Stage I AKIN injuries. In a proportion of these patients, renal function did not return to preoperative baseline at three months. Future studies are needed to elucidate whether this perioperative AKI kidney injury poses a risk for later development of more serious kidney dysfunction. Chronic health conditions, such as diabetes and hypertension, associated with the development of chronic kidney disease were also associated with an increased risk of postoperative AKI, as were blood transfusions and undergoing general anesthesia. Appreciation of these risk factors may lead to implementation of measures to avoid perioperative use of nephrotoxic agents and introduction of processes aimed at more stringent perioperative hydration and more routine postoperative renal function monitoring.
Notes
Over 95% of Mayo Clinic patients provided authorization for research use of their medical records.
References
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007; 89: 780-5.
Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am 2005; 87: 1487-97.
Mortazavi SM, Kakli H, Bican O, Moussouttas M, Parvizi J, Rothman RH. Perioperative stroke after total joint arthroplasty: prevalence, predictors, and outcome. J Bone Joint Surg Am 2010; 92: 2095-101.
van Klei WA, Bryson GL, Yang H, Forster AJ. Effect of beta-blocker prescription on the incidence of postoperative myocardial infarction after hip and knee arthroplasty. Anesthesiology 2009; 111: 717-24.
Kheterpal S, Tremper KK, Englesbe MJ, et al. Predictors of postoperative acute renal failure after noncardiac surgery in patients with previously normal renal function. Anesthesiology 2007; 107: 892-902.
Jafari SM, Huang R, Joshi A, Parvizi J, Hozack WJ. Renal impairment following total joint arthroplasty: who is at risk? J Arthroplasty 2010; 25: 49-53.
Aveline C, Leroux A, Vautier P, Cognet F, Le Hetet H, Bonnet F. Risk factors for renal dysfunction after total hip arthroplasty (French). Ann Fr Anesth Reanim 2009; 28: 728-34.
Berry DJ, Kessler M, Morrey BF. Maintaining a hip registry for 25 years. Mayo Clinic experience. Clin Orthop Relat Res 1997; 344: 61-8.
Alsara A, Warner DO, Li G, Herasevich V, Gajic O, Kor DJ. Derivation and validation of automated electronic search strategies to identify pertinent risk factors for postoperative acute lung injury. Mayo Clin Proc 2011; 86: 382-8.
Levey AS, Coresh J, Greene T, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med 2006; 145: 247-54.
Mehta RL, Kellum JA, Shah SV, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 2007; 11: R31.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42: 377-81.
Hosking MP, Warner MA, Lobdell CM, Offord KP, Melton LJ 3rd. Outcomes of surgery in patients 90 years of age and older. JAMA 1989; 261: 1909-15.
World Health Organization. Nutritional Anaemias. Report of a WHO Scientific Group. Geneva, 1968. Available from URL: http://whqlibdoc.who.int/trs/WHO_TRS_405.pdf (accessed September 2012).
Glance LG, Wissler R, Mukamel DB, et al. Perioperative outcomes among patients with the modified metabolic syndrome who are undergoing noncardiac surgery. Anesthesiology 2010; 113: 859-72.
Kheterpal S, Tremper KK, Heung M, et al. Development and validation of an acute kidney injury risk index for patients undergoing general surgery: results from a national data set. Anesthesiology 2009; 110: 505-15.
Chen J, Muntner P, Hamm LL, et al. The metabolic syndrome and chronic kidney disease in U.S. adults. Ann Intern Med 2004; 140: 167-74.
Murugan R, Kellum JA. Acute kidney injury: what’s the prognosis? Nat Rev Nephrol 2011; 7: 209-17.
Uchino S, Bellomo R, Goldsmith D, Bates S, Ronco C. An assessment of the RIFLE criteria for acute renal failure in hospitalized patients. Crit Care Med 2006; 34: 1913-7.
Mangano CM, Diamondstone LS, Ramsay JG, Aggarwal A, Herskowitz A, Mangano DT. Renal dysfunction after myocardial revascularization: risk factors, adverse outcomes, and hospital resource utilization. The Multicenter Study of Perioperative Ischemia Research Group. Ann Intern Med 1998; 128: 194-203.
Bove T, Calabro MG, Landoni G, et al. The incidence and risk of acute renal failure after cardiac surgery. J Cardiothorac Vasc Anesth 2004; 18: 442-5.
Coselli JS, Bozinovski J, LeMaire SA. Open surgical repair of 2286 thoracoabdominal aortic aneurysms. Ann Thorac Surg 2007; 83: S862-4.
Bihorac A, Yavas S, Subbiah S, et al. Long-term risk of mortality and acute kidney injury during hospitalization after major surgery. Ann Surg 2009; 249: 851-8.
Pavone V, Johnson T, Saulog PS, Sculco TP, Bottner F. Perioperative morbidity in bilateral one-stage total knee replacements. Clin Orthop Relat Res 2004; 421: 155-61.
Grundy SM, Brewer HB, Cleeman JI, Smith SC, American Heart Association, National Heart, Lung, and Blood Institute. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 2004; 109: 433-8.
Anfossi G, Russo I, Doronzo G, Trovati M. Relevance of the vascular effects of insulin in the rationale of its therapeutical use. Cardiovasc Hematol Disord Drug Targets 2007; 7: 228-49.
Abu-Saleh N, Ovcharenko E, Awad H, et al. Involvement of the endothelin and nitric oxide systems in the pathogenesis of renal ischemic damage in an experimental diabetic model. Life Sci 2012; DOI:10.1016/j.lfs.2012.02.002.
Kao MP, Ang DS, Pall A, Struthers AD. Oxidative stress in renal dysfunction: mechanisms, clinical sequelae and therapeutic options. J Hum Hypertens 2010; 24: 1-8.
Scott NB, Turfrey DJ, Ray DA, et al. A prospective randomized study of the potential benefits of thoracic epidural anesthesia and analgesia in patients undergoing coronary artery bypass grafting. Anesth Analg 2001; 93: 528-35.
Suleiman MY, Passannante AN, Onder RL, Greene-Helms WF, Perretta SG. Alteration of renal blood flow during epidural anesthesia in normal subjects. Anesth Analg 1997; 84: 1076-80.
Plataki M, Kashani K, Cabello-Garza J, et al. Predictors of acute kidney injury in septic shock patients: an observational cohort study. Clin J Am Soc Nephrol 2011; 6: 1744-51.
Karkouti K, Wijeysundera DN, Yau TM, et al. Acute kidney injury after cardiac surgery: focus on modifiable risk factors. Circulation 2009; 119: 495-502.
Karkouti K, Wijeysundera DN, Yau TM, et al. Influence of erythrocyte transfusion on the risk of acute kidney injury after cardiac surgery differs in anemic and nonanemic patients. Anesthesiology 2011; 115: 523-30.
Haase M, Bellomo R, Story D, et al. Effect of mean arterial pressure, haemoglobin and blood transfusion during cardiopulmonary bypass on post-operative acute kidney Injury. Nephrol Dial Transplant 2011; 27: 153-60.
Zufferey P, Merquiol F, Laporte S, et al. Do antifibrinolytics reduce allogeneic blood transfusion in orthopedic surgery? Anesthesiology 2006; 105: 1034-46.
Murray MD, Brater DC. Renal toxicity of the nonsteroidal anti-inflammatory drugs. Annu Rev Pharmacol Toxicol 1993; 33: 435-65.
Toto RD, Anderson SA, Brown-Cartwright D, Kokko JP, Brater DC. Effects of acute and chronic dosing of NSAIDs in patients with renal insufficiency. Kidney Int 1986; 30: 760-8.
Lee A, Cooper MG, Craig JC, Knight JF, Keneally JP. Effects of nonsteroidal anti-inflammatory drugs on postoperative renal function in adults with normal renal function. Cochrane Database Syst Rev 2007; (2): CD002765.
Carmichael J, Shankel SW. Effects of nonsteroidal anti-inflammatory drugs on prostaglandins and renal function. Am J Med 1985; 78: 992-1000.
Chawla LS. Acute kidney injury leading to chronic kidney disease and long-term outcomes of acute kidney injury: the best opportunity to mitigate acute kidney injury? Contrib Nephrol 2011; 174: 182-90.
Funding
This project was supported by the Department of Anesthesiology, College of Medicine, Mayo Clinic, Rochester, MN, 55905, and NIH/NCRR CTSA Grant Numbers UL1 RR024150 and KL2 RR024151. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Toby N. Weingarten wrote the manuscript. Toby N. Weingarten, Carmelina Gurrieri, Paul D. Jarett, Deforest R. Brown, Novette J. Berntson, Reynaldo D. Calaro, Daryl J. Kor, Daniel J. Berry, Vesna D. Garovic, Wayne T. Nicholson, Darrell R. Schroeder, and Juraj Sprung helped design the study, conduct the study, and analyze the data.
Rights and permissions
About this article
Cite this article
Weingarten, T.N., Gurrieri, C., Jarett, P.D. et al. Acute kidney injury following total joint arthroplasty: retrospective analysis. Can J Anesth/J Can Anesth 59, 1111–1118 (2012). https://doi.org/10.1007/s12630-012-9797-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-012-9797-2