Abstract
DNA methylation variation at HP1BP3 and TTC9B is modified by estrogen exposure in the rodent hippocampus and was previously shown to be prospectively predictive of postpartum depression (PPD) when modeled in antenatal blood. The objective of this study was to replicate the predictive efficacy of the previously established model in women with and without a previous psychiatric diagnosis and to understand the effects of changing hormone levels on PPD biomarker loci. Using a statistical model trained on DNA methylation data from N=51 high-risk women, we prospectively predicted PPD status in an independent N=51 women using first trimester antenatal gene expression levels of HP1BP3 and TTC9B, with an area under the receiver operator characteristic curve (AUC) of 0.81 (95% CI: 0.69–0.92, p<5 × 10−4). Modeling DNA methylation of these genes in N=240 women without a previous psychiatric diagnosis resulted in a cross-sectional prediction of PPD status with an AUC of 0.81 (95% CI: 0.68–0.93, p=0.01). TTC9B and HP1BP3 DNA methylation at early antenatal time points showed moderate evidence for association to the change in estradiol and allopregnanolone over the course of pregnancy, suggesting that epigenetic variation at these loci may be important for mediating hormonal sensitivity. In addition both loci showed PPD-specific trajectories with age, possibly mediated by age-associated hormonal changes. The data add to the growing body of evidence suggesting that PPD is mediated by differential gene expression and epigenetic sensitivity to pregnancy hormones and that modeling proxies of this sensitivity enable accurate prediction of PPD.
Similar content being viewed by others
INTRODUCTION
Postpartum depression (PPD) affects between 10 and 20% of women (Josefsson et al, 2001; Miller, 2002; Pearlstein et al, 2009) and has significant effects on both mother and child (Breese McCoy, 2011; Cuijpers et al, 2008; Field, 2011; Hirst and Moutier, 2010; O’Hara, 2009; Soufia et al, 2010). Certain populations have higher rates of PPD including 30% in women with a history of depression and 52% of women with bipolar disorder (Viguera et al, 2011). A growing body of evidence indicates that increased sensitivity to gonadal hormone levels such as estrogen mediate the biological vulnerability to PPD. Early work by Bloch et al (2000) provided clear evidence that women with a previous history of PPD are sensitive to drastic hormonal changes, whereas more recent studies have demonstrated significant gene expression changes in estrogen-responsive genes of women at risk for PPD (Mehta et al, 2014). Work out of our laboratory also provided evidence for a PPD-specific increased sensitivity to estrogen on the epigenetic level (Guintivano et al, 2013a). We demonstrated that women at risk for PPD exhibit more DNA methylation changes at loci that are sensitive to epigenetic reprogramming in the mouse hippocampus, a brain region thought to be involved in mediating estrogen’s effects on mood (Walf, 2010). From this data set, we identified two biomarker loci (HP1BP3 and TTC9B) that were capable of prospectively predicting PPD in humans with an area under the receiver operator characteristic curve (AUC) of 82%. Importantly, DNA methylation of HP1BP3 was associated with a number of inflammatory cell-type elevations occurring in assayed antenatally depressed relative to antenatally euthymic women (Guintivano et al, 2013a) and required incorporation of cellular heterogeneity metrics into the model to achieve an accurate prediction across both subgroups.
Bioinformatic analysis suggests that HP1BP3 and TTC9B may be involved in mediating synaptic plasticity (Guintivano et al, 2013a), a key facet of the antidepressant properties of estradiol in the hippocampus (ter Horst, 2010) and potentially of high relevance to susceptibility to PPD. We believe the predictive efficacy of the biomarker model lies in the ability of relative epigenetic differences in these estrogen-responsive genes to model PPD-associated sensitivity to estrogens. Of course, the estrogens are not the only reproductive hormones that undergo marked changes during pregnancy and the postpartum period. Progesterone and its metabolites also change considerably. Some studies in the past have indicated that progesterone withdrawal may be associated with PPD (Harris et al, 1994). Recent work has focused on allopregnanolone, one of progesterone’s 3α-reduced metabolites and a strong allosteric modulator of the GABA-A receptor (Bali and Jaggi, 2014; Bristot et al, 2014; Schumacher et al, 2014). It is therefore also possible that our biomarker model may be associated with changes in progesterone or allopregnanolone.
The objectives of this study were to independently replicate our previously published PPD prediction model in women with and without a prior psychiatric history, to further investigate the DNA methylation status of PPD biomarker loci with changing pregnancy hormone levels and over periods of major hormonal change.
MATERIALS AND METHODS
Human Samples
Subjects derived from two prospective cohorts designed to study PPD and two cohorts where DNA was taken long after pregnancy. The prospective cohorts included the Johns Hopkins Prospective PPD sample reported on previously by our group (Guintivano et al, 2013a) and a Prospective Gene Expression PPD cohort generated by Mehta et al (2014), which is a study investigating gene expression in pregnant women prospectively followed until they do or do not develop PPD. Both prospective cohorts were performed in women with previous diagnoses of mood disorder (Guintivano et al, 2013a; Mehta et al, 2014). The Franconian Maternal Health Evaluation Studies (FRAMES) cohort focused on psychiatrically healthy women with prospective evaluation of depression and blood drawn for DNA at 1–3 years postpartum. The Generations of Recurrent Early Onset Depression (GenRED) cohort involved retrospective symptom assessment and blood draws. Detailed information on study subjects is available below and in Table 1,Supplementary Table S1.
Johns Hopkins prospective PPD cohort
We recruited 93 pregnant women with a history of either Major Depression or Bipolar Disorder (I, II, or NOS) and prospectively followed them during pregnancy and after delivery to identify genetic and clinical characteristics that precede the development of a postpartum depressive episode. Approximately one-third of the sample had bipolar disorder. The average age of the participants was 30.6±6.3 and 70% of the sample was Caucasian. Participants were managed by their treating psychiatrist as clinically indicated and were evaluated during each trimester of pregnancy and then 1 week, 1 month, and 3 months postpartum. Women were classified as being depressed if they met DSM-IV criteria for a major depressive episode (MDE) based on a psychiatric interview at each time point (first, second, and third trimester and 1 week and 1 month postpartum). Childhood sexual abuse status was binarily coded as a response to the question ‘Were you sexually assaulted as a child?’ during a clinical interview. Although serum hormone levels were obtained longitudinally from multiple time points, blood was drawn for DNA analysis at only one time point per individual in this cohort. The trimester of blood draw is depicted in Supplementary Table S1. Prospective human subjects research at Johns Hopkins was conducted under IRB protocol # 00008149.
Prospective gene expression PPD cohort
Data from this cohort was generated by Mehta et al (2014) and was downloaded from the Gene Expression Omnibus (GEO) (http://www.ncbi.nlm.nih.gov/geo/) under accession number GSE45603. Subjects reportedly derived from a longitudinal cohort recruited at the Emory Women’s Mental Health Program. The sample was 33-year-old on average and ~85% Caucasian. Approximately 59.6 and 40.4% of the sample had a diagnosis of MDD and bipolar disorder, respectively, based on the Structured Clinical Interview for DSM-IV Axis I Disorders. Depressive symptoms were assessed in the first and third trimester using the Beck Depression Inventory, the 17-item Hamilton Depression Rating Scale (HDRS), and the Edinburgh Postnatal Depression Scale. Depression diagnoses in the first trimester and postpartum are based on the HDRS score >14, which represents the score on this scale demonstrated to be maximally predictive of experiencing a MDE in the postpartum period (Ji et al, 2011).
GenRED cohort
The retrospective sample derived from the GenRED cohort at Johns Hopkins consisting 84 women non-menopausal aged was 39.7±0.093 years at the time of blood draw. Data derived from EBV transformed lymphoblasts from women who had had a pregnancy. The sample was 92% Caucasian, 1.2% African American, 1.2% Asian, and 3.6% unreported. The menstrual cycle status at the time of blood sampling was not recorded. The frequency of psychiatric diagnosis was 44.6% major depressive disorder (MDD), 2.4% bipolar disorder type II, and 49% with no diagnosis. PPD in this cohort consisted of women who retrospectively reported experiencing depression in the postpartum period. Women experiencing depression symptoms antenatally that became euthymic during the postpartum period were classified as controls. Details on antenatal and PPD frequency per cohort are displayed in Table 1. Collection of the GenRED sample was performed under IRB protocol # 00035775.
FRAMES cohort
DNA was obtained from a subset of 421 women enrolled in the FRAMES and who were evaluated for genetic associations with postpartum outcomes in previous studies (Mehta et al, 2012). Of these samples, a total of N=240 passed quality control following subsequent analyses. All women were Caucasian and the mean age of the sample was 32.7±0.018 years. Women responded to the HDRS prospectively during the third trimester, between 48–72 h, and between 6–8 months after parturition and PPD was classified as scores >14. It has been demonstrated that a score of 14 or higher on the HDRS is ~ 80% sensitive and specific to identify the presence of a MDE as determined by SCID in both the early and late postpartum period (Ji et al, 2011). All blood drawn for this study ranged in age between 1–3 years after parturition. The menstrual cycle status at the time of blood sampling was not recorded. The study was approved by the Ethics Committee at Erlangen University Hospital, Nuremberg, Germany. All participants received detailed information and provided written consent. Human subjects research in this population at Johns Hopkins was performed under IRB protocol # 00049309.
Illumina HM450 Microarray Data
Genome-wide DNA methylation data generated on the Illumina Human Methylation 450 (HM450) bead array were generated in 51 women from the Women’s Mood Disorder Prospective sample previously (Guintivano et al, 2013a). Data can be found on the GEO (http://www.ncbi.nlm.nih.gov/geo/) under accession number GSE44132. DNA methylation helps to define cell types and as such, variation in cellular composition in heterogeneous tissues such as blood has the potential to bias study results if not appropriately corrected for (Guintivano et al, 2013b). As previously published, cell sub-fraction percentages were quantified for CD8-T cells, CD4-T cells, B cells, monocytes, and granulocytes by inputting DNA methylation signatures of 473 loci into an algorithm designed for quantification of the cell types using DNA methylation proxies (Houseman et al, 2012).
Sodium Bisulfite Pyrosequencing
Bisulfite conversion was carried out using EZ DNA Methylation Gold Kit (Zymo Research, Irvine, CA) according to the manufacturer’s instructions. Nested PCR amplifications were performed with a standard PCR protocol in 25 μl volume reactions containing 3–4 μl of sodium-bisulfite-treated DNA, 0.2 μM primers, and master mix containing Taq DNA polymerase (Sigma Aldrich, St Louis, MO). Primer sequences can be found in Supplementary Table S2. PCR amplicons were processed for pyrosequencing analysis according to the manufacturer’s standard protocol (QIAGEN, Germantown, MD) using a PyroMark MD system (QIAGEN) with Pyro Q-CpG 1.0.9 software (QIAGEN) for CpG methylation quantification.
Gene Expression Data
Gene expression data generated on the Illumina HumanHT-12 V4.0 expression beadchip by Mehta et al (2014) was downloaded from GEO accession GSE45603. Raw data were normalized with the variance stabilizing transformation method (Huber et al, 2002) using the ‘justvsn’ function from the vsn package in R. Relative gene expression values for HP1BP3 and TTC9B were extracted from the normalized data set for subsequent analysis. We quantified the relative proportions of CD8-T, CD4-T, B cell, monocyte, and granulocyte proportions using the CellMix package in R (Gaujoux and Seoighe, 2013) based on reference data in 42 probes available in both GSE45603 and those available in the reference data set generated by Abbas et al (2009).
Hormone Data
Participant blood was collected at each visit in four 10 ml EDTA tubes and were immediately centrifuged at 4 °C for 30 min. The serum was then aliquoted into 2 ml microcentrifuge tubes, snap frozen on dry ice, and immediately stored in a −80 °C freezer. The blood samples we chose for analysis were from women who had data for at least one antepartum blood draw and one postpartum visit with psychological data. Blood was analyzed with the following kits: Allopregnanolone EIA kit from Arbor Assays LLC (Ann Arbor, MI, USA) Cat 3 KC44-H1, Progesterone EIA kit from Alpco (Salem, NH, USA) catalog # PROHU-E01, Estradiol Alpco Elisa kit catalog number 11ESPHU-E 1.
Statistical Analysis
All statistical tests were performed in R (http://www.r-project.org/). Using an Anderson–Darling test from the nortest package, all distributions of data that rejected the null hypothesis of normality were subsequently evaluated with non-parametric tests. All statistical tests performed were two tailed and a p<0.05 is considered significant. Unless otherwise specified±denotes the SEM.
PPD prediction for all cohorts was achieved using the previously published model (Guintivano et al, 2013a):

Where PPD status for individual (i) was modeled as a function of an interaction of HP1BP3 DNA methylation with cell-type variable (j), where j is the ratio of monocyte to non-monocyte counts (See Method S1 for relevant rationale), controlling for additive covariate TTC9B DNA methylation. To apply our DNA methylation model to gene expression scores when applied to the Prospective Gene Expression cohort, we rebuilt the training set-derived model from the Johns Hopkins Prospective Cohort after first converting DNA methylation at HP1BP3 and TTC9B to z-scores in order to standardize the variation between the two loci relative to each other (Supplementary Figure S1). For the FRAMES cohort, cell-type information was not available and was not controlled for. Similar to results reported by Mehta et al (2014), psychiatric medication status did not influence PPD prediction model performance in the Johns Hopkins Prospective PPD cohort and were not included in subsequent analyses (Supplementary Result S1).
Sliding window analysis was used in the investigation of age-related changes to DNA methylation, whereby DNA methylation values for each gene were averaged for all women within 5 years of age for each age between 25 and 50.
RESULTS
Independent Prospective Replication of our PPD Predictive Model in Women with Mood Disorder
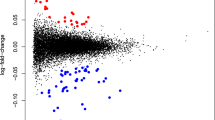
We attempted to apply our PPD biomarker model to the Prospective Gene Expression cohort generated by Mehta et al (2014) across multiple time points during pregnancy. Input of gene expression z-scores generated for HP1BP3 (ILMN_1701169) and TTC9B (ILMN_1682123) and the monocyte to non-monocyte ratio generated significant predictions for PPD from first trimester but not third trimester blood (Figure 1, Table 1). Incorporation of cell-type ratio into the model as an interacting factor was necessary for accurate PPD prediction across antenatally euthymic and depressed women (Supplementary Result S2, Supplementary Figure S2). The predictive accuracy from first trimester blood was similar ~80% when modeling only PPD cases deriving from antenatally euthymic or depressed women separately (Table 1), whereas third trimester-derived predictions were not significant (Table 1). Permutation analysis of each model component separately was employed to understand model factors contributing to predictive efficacy. Both TTC9B and HP1BP3 gene expression significantly contributed to model performance in the antenatally euthymic and combined sample for the first trimester time point.
Receiver operator characteristic curves of prospective PPD prediction. Receiver Operator Characteristic (ROC) curves depicting the sensitivity (y axis) as a function of specificity (x axis) for prediction of PPD status in the Prospective Gene Expression cohort during the first (a) and third (b) trimesters.
Unlike our originally published study, no significant associations of the monocyte to non-monocyte ratio were observed with antenatal depression status; however, a non-significant decrease was observed at the first trimester time point (Wilcoxon Rank Sum Test, PPD=0.24+0.0067, non-PPD=0.23+0.0021, p=0.085), suggesting that antenatal depression-associated variation in cell type may be driving the improved predictability of the model during this time point. Indeed, application of an alternative model trained on the Johns Hopkins Prospective cohort but lacking the interacting cell-type ratio covariate generates a lower AUC of 0.75 (95% CI: 0.6–0.88, Model P=0.001, HP1BP3 P=0.78, TTC9B P=0.0099) and permutation analysis reveals that the HP1BP3 component is no longer significantly contributing to the predictive efficacy.
Independent Replication of PPD Predictive Model in Women with no Previous Psychiatric History
PPD model efficacy was assessed for the ability to detect women with HDRS scores above 14 at 6–8 month postpartum in a cohort of women with no previous history of psychiatric diagnosis. Women with high HDRS scores at 2–3 day postpartum were excluded, as high HDRS scores at this time may be associated with more standard pregnancy-related mood fluctuations. The PPD prediction model generated a significant AUC of 81% in this cohort (Figure 3a, Table 1). Similar to the other DNA methylation models, both HP1BP3 and TTC9B significantly contributed to model performance (Table 1). Prediction accuracy in the FRAMES cohort increased in sensitivity, specificity, and significance with increasing severity of depression scores in the postpartum period (Figure 2b, Supplementary Table S3).
PPD prediction in women without a psychiatric history. (a) Receiver operator characteristic (ROC) curves depicting the sensitivity (y axis) as a function of specificity (x axis) for prediction of 6–8 months HDRS scores ⩾14 status in the FRAMES cohort of women from the general population. (b) A plot of the performance of PPD model prediction as measured by AUC (y axis) as a function of the HDRS cutoff signifying affected individuals (x axis). The horizontal line denotes the threshold of a ‘good’ biomarker at an AUC of 0.80, whereas the vertical dashed line denotes an HDRS cutoff of 14.
Age as a Macro Model of Hormone Withdrawal
We used the GenRED sample to assess the change in DNA methylation in PPD biomarker loci over time. Using a sliding window analysis, women with a history of PPD showed significantly anti-correlated trajectories to non-PPD women as a function of age for HP1BP3 (Rho=−0.5, p=0.006) and TTC9B (Rho=−0.8, p=1.8 × 10−7) (Figure 3). The same sliding window analysis employed in the FRAMES cohort identified similar anti-correlated trajectories between PPD and non-PPD women for HP1BP3 (Rho=−0.65, p=7.1 × 10−4) and TTC9B (Rho=−0.65, p=7.8 × 10−4) (Figure 3).
PPD biomarkers across the reproductive years. Plots of the mean DNA methylation (x axis) for PPD (triangles) and non-PPD (circles) cases for the HP1BP3 (a) and TTC9B (b) genes over a 10-year sliding window as a function of age (y axis) in the GenRED cohort. Plots of the mean DNA methylation (x axis) for PPD (triangles) and non-PPD (circles) cases for the HP1BP3 (c) and TTC9B (d) genes over a 10-year sliding window as a function of age (y axis) in the FRAMES cohort. The vertical dashed line represents an age of 35 years and denotes the approximate age in the female population when estrogen levels begin to decline.
Association of PPD Biomarker Loci with Hormone Levels
HP1BP3 and TTC9B DNA methylation levels were assessed for association to serum hormone levels of estradiol, progesterone, and allopregnanolone during the second and third trimester in the Johns Hopkins Prospective cohort. No relationship was observed between the number of live births per subject and gonadal hormone levels or PPD biomarker loci (Supplementary Result S3). As hormone levels varied as a function of gestational age (Supplementary Figure S3), linear models adjusting for the change in gestational age per individual were employed to control for associations owing to variation in sampling time. No significant associations were observed between HP1BP3 and any of the investigated hormones, whereas TTC9B DNA methylation was positively correlated with third trimester levels of estradiol (β=0.0058±0.0021, F=4.8, df=2/26, p=0.01) (Figure 4a). When we divided the cohort by depression status at the third trimester, this effect remained significant in women who were antenatally euthymic (β=0.0058±0.0026, F=4.39, df=2/16, p=0.038), but not in those who were antenatally depressed (β=0.0033±0.0045, F=0.48, df=2/7, p=0.49). In an effort to assess the directionality of the observed association, we assessed third trimester estradiol levels as a function of second trimester TTC9B DNA methylation and observed a non-significant positive association in antenatally euthymic women (β=0.0093±0.0042, F=2.74, df=2/7, p=0.061) that was markedly weakened when assessing the combined sample of antenatally euthymic and depressed women together (β=0.0057±0.0037, F=1.43, df=2/11, p=0.15). We next assessed the change in hormone levels from second to third trimester time points to rule out an association with a pre-existing hormonal state. We observed a similar relationship of estradiol to TTC9B methylation in antenatally euthymic women when assessing the change in estradiol levels from second to third trimester (β=0.0087±0.0043, F=2.13, df=2/8, p=0.078) (Figure 4b) that was weakened by the addition of antenatally depressed subjects (β=0.0057±0.0036, F=1.36, df=2/12, p=0.13). Notably, second trimester estradiol levels were not associated with second trimester TTC9B DNA methylation (β=0.0005±0.0026, F=0.039, df=1/14, p=0.85).
PPD biomarkers and pregnancy hormone trajectories. (a) A scatterplot of the third trimester estradiol levels in (y axis) as a function of TTC9B DNA methylation (x axis) for women who did (triangles, dashed regression line) and did not (circles, solid regression line) develop PPD. (b) A scatterplot of the change in estradiol from second to third trimester (y axis) as a function of second trimester TTC9B DNA methylation levels (x axis) for women who did (triangles, dashed regression line) and did not (circles, solid regression line) develop PPD. (c) A scatterplot of the third trimester allopregnanolone levels in (y axis) as a function of HP1BP3 DNA methylation (x axis) for women who did (triangles, dashed regression line) and did not (circles, solid regression line) develop PPD. (d) A scatterplot of the change in allopregnanolone from second to third trimester (y axis) as a function of second trimester HP1BP3 DNA methylation levels (x axis) for women who did (triangles, dashed regression line) and did not (circles, solid regression line) develop PPD. All data derives from the Johns Hopkins Prospective cohort.
In light of the observed moderate evidence that epigenetic variation at earlier time points may associate with the trajectory of hormonal changes during pregnancy, we re-evaluated HP1BP3 DNA methylation levels in association with the change in hormone levels. Third trimester allopregnanolone was not associated with HP1BP3 DNA methylation (Rho=−0.17, p=0.32) (Figure 4c); however, as in the case with TTC9B DNA methylation and estradiol, second trimester HP1BP3 DNA methylation was associated with third trimester allopregnanolone levels in antenatally euthymic women (β=−0.36±0.12, F=5.18, df=2/5, p=0.026) but not in the combined sample (β=−0.29±0.21, F=1.94, df=2/10, p=0.18). In addition, significant negative associations were observed for the change in allopregnanolone levels from second to third trimester in the antenatally euthymic (β=−0.46±0.14, F=8.35, df=2/5, p=0.022) (Figure 4d) but not antenatally depressed samples (β=−0.33±0.30, F=1.85, df=2/10, p=0.3). As was the case with our findings concerning TTC9B and estradiol, is it notable that the primary effect appears to be derived from the antenatally euthymic group (Supplementary Figure S4). To corroborate these findings, an exploratory analysis in the Prospective Gene Expression cohort found evidence for an overrepresentation of third trimester allopregnanolone associated loci with first trimester HP1BP3 expression but not third trimester HP1BP3 expression (Supplementary Result S4, Supplementary Figure S5A). Similarly, first trimester but not third trimester TTC9B gene expression was associated with third trimester estradiol-associated loci (Supplementary Result S4, Supplementary Figure S5B).
DISCUSSION
Using gene expression values in an independent prospective cohort of 51 women, our model prospectively predicted PPD with a similar accuracy to our original report at ~80%, suggesting that our model remains a valid predictor of future PPD risk. The success of the model in a gene expression sample despite being trained on a DNA methylation sample suggests that epigenetic variation at PPD biomarker loci is likely to be associated with expression. This supposition is corroborated by the observation of an association with monocyte to non-monocyte ratio with HP1BP3 gene expression in a direction similar to that observed for DNA methylation in the original study. As the regions of relevant epigenetic change in HP1BP3 and TTC9B reside within or proximal to the promoters for each gene, it is not unreasonable to assume that there may be a relationship to blood gene expression; however, this should be assessed in future studies as we lacked a data set to evaluate this specifically. Future studies should investigate if epigenetic variation at HP1BP3 and TTC9B can be mediated by genetic variation as has been observed for other epigenetic associations with PPD (Bell et al, 2015).
The original report by Mehta et al did not incorporate a metric of cellular heterogeneity and was reportedly unable to predict PPD status in those women with antenatal depression, whereas our model appeared to function similarly in antenatally euthymic and depressed women, possibly owing to the incorporation of cell-type ratio information. Permutation analyses demonstrated that HP1BP3 contributed significantly to the prediction of PPD in antenatally euthymic but not antenatally depressed women. We further demonstrated that application of an alternative model lacking the interacting cell-type ratio eliminated the ability of HP1BP3 variation to contribute significantly to the predictive efficacy of our model. Taken together, the data corroborate the previously published data (Guintivano et al, 2013a), indicating that changes in cell-type ratio may confound the association of HP1BP3 to PPD status and must be carefully controlled for in future studies. Unlike our original study, however, cellular heterogeneity demonstrated only moderate evidence for association with antenatal depression status in the gene expression cohort, suggesting that there are likely other factors not accounted for in our model that distinguish depression that continues into the postpartum period from depression arising only postpartum; these may be of critical importance for improving the predictive capacity of the model. In the Johns Hopkins Prospective cohort, direct assessment of hormone levels indicated that DNA methylation at earlier time points was indicative of the levels of estradiol and allopregnanolone for TTC9B and HP1BP3, respectively, and these data were stronger in antenatally euthymic as compared with antenatally depressed women. Together these results suggest that women developing PPD who were euthymic during pregnancy may have unique hormonal milieu relative to those depressed during pregnancy.
Importantly, these prospectively assessed hormone associations argue for a contributing role of epigenetic variation to the etiology of varying hormone levels as opposed to being merely an effect of hormonal sensitivity; however, a robust replication of these findings in larger cohorts and functional studies are warranted to support this claim. Such a role may explain why the PPD prediction model generated by Mehta et al (2014), on this data set was most predictive during the third trimester, whereas our model performed best during the first trimester. Mehta et al’s model was enriched for estrogen receptor target genes, which may exhibit the most prominent differences during the third trimester when levels of pregnancy-associated estrogens are highest. Alternatively, HP1BP3 and TTC9B variation at earlier time points may be more important not only for reflecting PPD-associated hormonal sensitivity but potentially for contributing to later time point hormonal outcomes. Notably, application of these two genes to PPD prediction in the originally published DNA methylation sample demonstrated similar predictive efficacies independent of the antenatal time point at which blood was drawn (Guintivano et al, 2013a), suggesting the trimester-specific limitation on predictive efficacy may be specific to gene expression studies.
The observed associations of PPD biomarker loci with hormone changes corroborates previously reported bioinformatic evidence, suggesting both TTC9B and HP1BP3 may be involved in modulating hippocampal synaptic plasticity (Guintivano et al, 2013a). Neither TTC9B nor HP1BP3 have extensive evidence regarding their gene functions that may be of etiological relevance to PPD. Both genes have ties to estrogen signaling. TTC9B expression has been shown to be responsive to gonadal hormones (Cao et al, 2006) and is discussed in depth below. HP1BP3 associates with ERβ in culture (Nassa et al, 2011), binds to chromatin specifically at the repressive histone 3 lysine 9 trimethylation (H3K9me3) mark, and is expressed in most tissues with 10-fold higher levels in the brain (Garfinkel et al, 2015). Knockdown of HP1BP3 by siRNA in culture leads to significant expression changes in hundreds of genes, suggesting it is involved in transcriptional regulation (Dutta et al, 2014; Garfinkel et al, 2015). Interestingly, some genes with the most significantly altered expression in culture experiments are known to mediate progesterone inhibition of estradiol signaling in the uterus, such as MIG-6 (Yoo et al, 2015). Of those 12 loci consistently affected by HP1BP3 knockdown in both of the above studies, three may have implications for mood. ITGA6 is downregulated in a chronic mild stress-based depression paradigm in rodents (Orsetti et al, 2008), EIF4B is implicated in mTOR signaling of relevance for depression (Jernigan et al, 2011), and GLO1 is implicated in BDNF signaling (Karpova et al, 2014), a downstream consequence of estrogen signaling in the hippocampus. Murine knockout of HP1BP3 leads to growth retardation (Garfinkel et al, 2015), further suggesting a possible role for modulation of trophic factors in the context of the brain. Although the conclusions regarding brain-specific function of HP1BP3 DNA methylation variation are limited at this time and must be interpreted with caution, the available data to date suggest a relationship with mood, mediated by either by downstream gene expression changes or neurosteroid levels, may be possible and warrants further study.
A contribution of HP1BP3 variation to allopregnanolone levels is one way by which this gene may affect mood. The considerable animal research on the anxiolytic effects of allopregnanolone has been summarized by Schule et al (2014). Significant research links low levels of allopregnanolone to depressed mood (Backstrom et al, 2014; Eser et al, 2006; Le Melledo and Baker, 2004; Padberg et al, 2002; Pinna et al, 2006; Schule et al, 2014; Strohle et al, 1999; Uzunova et al, 2006) and other evidence links mood states or histories thereof with alterations in the ratio of allopregnanolone to its precursors (Girdler et al, 2012; Schiller et al, 2014). In the perinatal period specifically, Deligiannidis et al (2013), in a small sample, found no relationship between pregnancy allopregnanolone and the development of PPD, whereas Hellgren et al (2014) found significantly lower levels of allopregnanolone in depressed pregnant women when compared with healthy controls (Hellgren et al, 2014). In a separate analysis, our group found that low levels of allopregnanolone measured in the second trimester predicted the development of PPD (p=0.01); this effect was driven by women who were euthymic in the second trimester (Osborne et al, under review).
The effects of estradiol on hippocampally mediated mood are widely supported by estrogen receptor knockout experiments (Walf et al, 2008), 17β-estradiol administration experiments (Osterlund et al, 2005), and selective ER antagonists and agonists (Walf and Frye, 2005). Furthermore, estradiol administration has been shown to increase synaptic plasticity and dendritic spine density within the hippocampus (ter Horst, 2010), whereas withdrawal from pregnancy levels of estradiol results in decreased hippocampal BDNF expression (Suda et al, 2008) and suppressed hippocampal neurogenesis (Green and Galea, 2008). Finally, high as compared with low E2 doses may inhibit neurogenesis in the dentate gyrus (Tanaka and Sokabe, 2013), suggesting that PPD-associated estrogen sensitivity may have deleterious consequences on mood in at-risk women. As such, TTC9B would be expected to have numerous consequences on mood and hippocampal synaptic plasticity through an alteration of estrogen trajectories.
Corroborating the assertion that TTC9B variation may contribute to estrogen sensitivity, a recent study identified that a close homolog of TTC9B, namely TTC9A, functions to regulate estrogen receptor alpha (ERα) levels (Shrestha et al, 2015). Importantly, TTC9A and B are highly conserved and share all regulatory protein domains (Shrestha et al, 2015), suggesting that they may have functional similarities such that TTC9B may contribute to the sensitivity of estrogen signaling implicated in PPD. An important possibility requiring further study is that these loci may be involved in feedback inhibition, as another study suggested that TTC9A appeared to be a target of the ERα in mammary tissue (Shrestha et al, 2012) and previous research out of our laboratory and others implicates that in vitro and in vivo estradiol treatment alters TTC9B expression (Cao et al, 2006) and methylation (Guintivano et al, 2013a), respectively.
A feedback regulation mechanism may reconcile the PPD-specific age-related trajectories of TTC9B and HP1BP3 methylation with the above data, implicating a possible causal role for these loci in contributing to hormonal sensitivity. For example, using data generated in the GenRED and FRAMES cohorts, we demonstrated that the trajectory of DNA methylation for PPD biomarker loci appeared to be reflective of the average levels of the estrogens over a woman’s life span and is significantly anti-correlated between PPD at risk and non-at risk women, further corroborating the assertion that their biomarker efficacy is based on their ability to be reflective of epigenetic sensitivity to estrogens. During the reproductive years, on average PPD biomarker loci appear to exhibit relative methylation differences similar to those observed in the antenatal period when estrogen levels are high, though they may vary with fluctuations as a result of the menstrual cycle not detectable in our data. However, as estrogen levels drop after age ~35, relative DNA methylation levels at HP1BP3 and TTC9B at risk women begin to diverge in the opposite direction between PPD and non-PPD and speaks to what may be observed for these loci in the postpartum period. An intriguing possibility warranting further study is that PPD biomarker epigenetic variation may be predictive of other female-specific mood disorders such as perimenopausal depression. Three out of four studies have observed significant associations between postpartum mood symptoms and perimenopausal depressive symptoms (Payne et al, 2009). A caveat of this interpretation is that we did not measure estrogen levels with age and are basing this conclusion on the average levels of estrogen fluctuation in women. Other potential caveats are that PPD diagnoses in the GenRED samples are based on retrospective report; however, a replication of our observations in the FRAMES cohort where depression was derived prospectively supports the observations that differing epigenetic trajectories occur in women who will experience depression postpartum. Importantly, the data suggest that validation efforts of PPD biomarker model prediction may be possible in retrospective blood samples taken from women who have experienced PPD.
Such validation efforts did appear possible in the FRAMES cohort, where application of the PPD biomarker prediction model demonstrated a high ability to identify women exhibiting depressive symptoms at 6 months postpartum. We focused on this time period to avoid classifying incidences of ‘baby blues’ (Breese McCoy, 2011) as PPD. Critically, unlike our original study and the data set generated by Mehta et al, these results demonstrate that our model may be efficacious in a general population sample without a history of mood disorder. It is of note that only a small number (2.1%) of women developed depressive symptoms postpartum compared with the reported averages of 10–20% (Josefsson et al, 2001; Miller, 2002; Pearlstein et al, 2009). Permutation analyses increase the confidence that the high AUC values observed are not a result of small numbers of cases. Interestingly, the possible fluctuation of gonadal hormone levels as a function of normal menstrual cycling did not appear to affect our predictive accuracy. The reasons for this are unclear and may be related to either the low levels of normal cycling relative to pregnancy level hormones at the measured time point or the timing of epigenetic change in response to hormonal variation, both of which should be evaluated in future studies. Notably, accounting for cell-type variation was not necessary to enable accurate prediction in the FRAMES cohort, possibly because DNA was derived from blood taken long after pregnancy and was no longer influenced by inflammatory cell-type changes at the time of measurement.
In conclusion, our study provides two independent replications of the predictive efficacy of our PPD biomarker model in both a high risk and general population sample and provides additional evidence of the potential functional relevance of HP1BP3 and TTC9B to disease etiology. In light of the devastating impact of PPD on both mothers and their children (Breese McCoy, 2011; Cuijpers et al, 2008; Field, 2011; Hirst and Moutier, 2010; O’Hara, 2009; Soufia et al, 2010), the epigenetic PPD biomarker may facilitate efforts by a growing number of states to implement early screening and intervention for PPD.
FUNDING AND DISCLOSURE
Drs Kaminsky and Payne are co-inventors listed on a patent application for DNA methylation at biomarker loci related to PPD. Dr Kaminsky is listed on patents for use of epigenetic information at the SKA2 locus to predict suicidal behavior and PTSD and received consultant fees from Janssen Research and Development, LLC. This work was funded in part by a NARSAD 2010 Young Investigator Award to Dr Kaminsky and by National Institute of Mental Health (NIMH) Grants R01MH059552 to Dr Goes and K23 MH074799-01A2 to Dr Payne. Dr Payne received legal consulting fees from Pfizer, Astra Zeneca and Johnson and Johnson and research support from Corcept Therapeutics. Family of Dr Kimmel owns stock with Abbvie and Abbott Laboratories. Dr Binder is listed on patent applications related to FKBP5 and ABCB1 as predictors of antidepressant treatment response. Dr Fasching received consulting fees from Roche, Novartis, Teva and Genomic Health, received speaker’s honoraria from Amgen, Roche, Pfizer, Novartis, Genomic Health, Teva, and GSK, and received research grants from Amgen and Novartis. Family of MK owns stock with Abbvie and Abbott Laboratories. All other authors declare no biomedical financial interests or potential conflicts of interest.
References
Abbas AR, Wolslegel K, Seshasayee D, Modrusan Z, Clark HF (2009). Deconvolution of blood microarray data identifies cellular activation patterns in systemic lupus erythematosus. PloS One 4: e6098.
Backstrom T, Bixo M, Johansson M, Nyberg S, Ossewaarde L, Ragagnin G et al (2014). Allopregnanolone and mood disorders. Prog Neurobiol 113: 88–94.
Bali A, Jaggi AS (2014). Multifunctional aspects of allopregnanolone in stress and related disorders. Prog Neuropsychopharmacol Biol Psychiatry 48: 64–78.
Bell AF, Carter CS, Steer CD, Golding J, Davis JM, Steffen AD et al (2015). Interaction between oxytocin receptor DNA methylation and genotype is associated with risk of postpartum depression in women without depression in pregnancy. Front Genet 6: 243.
Bloch M, Schmidt PJ, Danaceau M, Murphy J, Nieman L, Rubinow DR (2000). Effects of gonadal steroids in women with a history of postpartum depression. Am J Psychiatry 157: 924–930.
Breese McCoy SJ (2011). Postpartum depression: an essential overview for the practitioner. South Med J 104: 128–132.
Bristot G, Ascoli B, Gubert C, Panizzutti B, Kapczinski F, Rosa AR (2014). Progesterone and its metabolites as therapeutic targets in psychiatric disorders. Expert Opin Ther Target 18: 679–690.
Cao S, Iyer JK, Lin V (2006). Identification of tetratricopeptide repeat domain 9, a hormonally regulated protein. Biochem Biophys Res Commun 345: 310–317.
Cuijpers P, Brannmark JG, van Straten A (2008). Psychological treatment of postpartum depression: a meta-analysis. J Clin Psychol 64: 103–118.
Deligiannidis KM, Sikoglu EM, Shaffer SA, Frederick B, Svenson AE, Kopoyan A et al (2013). GABAergic neuroactive steroids and resting-state functional connectivity in postpartum depression: a preliminary study. J Psychiatr Res 47: 816–828.
Dutta B, Ren Y, Hao P, Sim KH, Cheow E, Adav S et al (2014). Profiling of the chromatin-associated proteome identifies HP1BP3 as a novel regulator of cell cycle progression. Mol Cell Proteom 13: 2183–2197.
Eser D, Romeo E, Baghai TC, di Michele F, Schule C, Pasini A et al (2006). Neuroactive steroids as modulators of depression and anxiety. Neuroscience 138: 1041–1048.
Field T (2011). Prenatal depression effects on early development: a review. Infant Behav Dev 34: 1–14.
Garfinkel BP, Melamed-Book N, Anuka E, Bustin M, Orly J (2015). HP1BP3 is a novel histone H1 related protein with essential roles in viability and growth. Nucleic Acids Res 43: 2074–2090.
Gaujoux R, Seoighe C (2013). CellMix: a comprehensive toolbox for gene expression deconvolution. Bioinformatics 29: 2211–2212.
Girdler SS, Lindgren M, Porcu P, Rubinow DR, Johnson JL, Morrow AL (2012). A history of depression in women is associated with an altered GABAergic neuroactive steroid profile. Psychoneuroendocrinology 37: 543–553.
Green AD, Galea LA (2008). Adult hippocampal cell proliferation is suppressed with estrogen withdrawal after a hormone-simulated pregnancy. Horm Behav 54: 203–211.
Guintivano J, Arad M, Gould TD, Payne JL, Kaminsky ZA (2013a). Antenatal prediction of postpartum depression with blood DNA methylation biomarkers. Mol Psychiatry 19: 633.
Guintivano J, Aryee MJ, Kaminsky ZA (2013b). A cell epigenotype specific model for the correction of brain cellular heterogeneity bias and its application to age, brain region and major depression. Epigenetics 8: 290–302.
Harris B, Lovett L, Newcombe RG, Read GF, Walker R, Riad-Fahmy D (1994). Maternity blues and major endocrine changes: Cardiff puerperal mood and hormone study II. BMJ 308: 949–953.
Hellgren C, Akerud H, Skalkidou A, Backstrom T, Sundstrom-Poromaa I (2014). Low serum allopregnanolone is associated with symptoms of depression in late pregnancy. Neuropsychobiology 69: 147–153.
Hirst KP, Moutier CY (2010). Postpartum major depression. Am Fam Physician 82: 926–933.
Houseman EA, Accomando WP, Koestler DC, Christensen BC, Marsit CJ, Nelson HH et al (2012). DNA methylation arrays as surrogate measures of cell mixture distribution. BMC Bioinformatics 13: 86.
Huber W, von Heydebreck A, Sultmann H, Poustka A, Vingron M (2002). Variance stabilization applied to microarray data calibration and to the quantification of differential expression. Bioinformatics 18 (Suppl 1): S96–104.
Jernigan CS, Goswami DB, Austin MC, Iyo AH, Chandran A, Stockmeier CA et al (2011). The mTOR signaling pathway in the prefrontal cortex is compromised in major depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry 35: 1774–1779.
Ji S, Long Q, Newport DJ, Na H, Knight B, Zach EB et al (2011). Validity of depression rating scales during pregnancy and the postpartum period: impact of trimester and parity. J Psychiatr Res 45: 213–219.
Josefsson A, Berg G, Nordin C, Sydsjo G (2001). Prevalence of depressive symptoms in late pregnancy and postpartum. Acta Obstet Gynecol Scand 80: 251–255.
Karpova NN, Lindholm JS, Kulesskaya N, Onishchenko N, Vahter M, Popova D et al (2014). TrkB overexpression in mice buffers against memory deficits and depression-like behavior but not all anxiety- and stress-related symptoms induced by developmental exposure to methylmercury. Front Behav Neurosci 8: 315.
Le Melledo JM, Baker G (2004). Role of progesterone and other neuroactive steroids in anxiety disorders. Expert Rev Neurother 4: 851–860.
Mehta D, Newport DJ, Frishman G, Kraus L, Rex-Haffner M, Ritchie JC et al (2014). Early predictive biomarkers for postpartum depression point to a role for estrogen receptor signaling. Psychol Med 44: 1–14.
Mehta D, Quast C, Fasching PA, Seifert A, Voigt F, Beckmann MW et al (2012). The 5-HTTLPR polymorphism modulates the influence on environmental stressors on peripartum depression symptoms. J Affect Disord 136: 1192–1197.
Miller LJ (2002). Postpartum depression. JAMA 287: 762–765.
Nassa G, Tarallo R, Ambrosino C, Bamundo A, Ferraro L, Paris O et al (2011). A large set of estrogen receptor beta-interacting proteins identified by tandem affinity purification in hormone-responsive human breast cancer cell nuclei. Proteomics 11: 159–165.
O’Hara MW (2009). Postpartum depression: what we know. J Clin Psychol 65: 1258–1269.
Orsetti M, Di Brisco F, Canonico PL, Genazzani AA, Ghi P (2008). Gene regulation in the frontal cortex of rats exposed to the chronic mild stress paradigm, an animal model of human depression. Eur J Neurosci 27: 2156–2164.
Osterlund MK, Witt MR, Gustafsson JA (2005). Estrogen action in mood and neurodegenerative disorders: estrogenic compounds with selective properties-the next generation of therapeutics. Endocrine 28: 235–242.
Padberg F, di Michele F, Zwanzger P, Romeo E, Bernardi G, Schule C et al (2002). Plasma concentrations of neuroactive steroids before and after repetitive transcranial magnetic stimulation (rTMS) in major depression. Neuropsychopharmacology 27: 874–878.
Payne JL, Palmer JT, Joffe H (2009). A reproductive subtype of depression: conceptualizing models and moving toward etiology. Harv Rev Psychiatry 17: 72–86.
Pearlstein T, Howard M, Salisbury A, Zlotnick C (2009). Postpartum depression. Am J Obstet Gynecol 200: 357–364.
Pinna G, Costa E, Guidotti A (2006). Fluoxetine and norfluoxetine stereospecifically and selectively increase brain neurosteroid content at doses that are inactive on 5-HT reuptake. Psychopharmacology 186: 362–372.
Schiller CE, Schmidt PJ, Rubinow DR (2014). Allopregnanolone as a mediator of affective switching in reproductive mood disorders. Psychopharmacology 231: 3557–3567.
Schule C, Nothdurfter C, Rupprecht R (2014). The role of allopregnanolone in depression and anxiety. Prog Neurobiol 113: 79–87.
Schumacher M, Mattern C, Ghoumari A, Oudinet JP, Liere P, Labombarda F et al (2014). Revisiting the roles of progesterone and allopregnanolone in the nervous system: resurgence of the progesterone receptors. Prog Neurobiol 113: 6–39.
Shrestha S, Cao S, Lin VC (2012). The local microenvironment instigates the regulation of mammary tetratricopeptide repeat domain 9A during lactation and involution through local regulation of the activity of estrogen receptor alpha. Biochem Biophys Rese Commun 426: 65–70.
Shrestha S, Sun Y, Lufkin T, Kraus P, Or Y, Garcia YA et al (2015). Tetratricopeptide repeat domain 9A negatively regulates estrogen receptor alpha activity. Int J Biol Sci 11: 434–447.
Soufia M, Aoun J, Gorsane MA, Krebs MO (2010). SSRIs and pregnancy: a review of the literature. Encephale 36: 513–516.
Strohle A, Romeo E, Hermann B, Pasini A, Spalletta G, di Michele F et al (1999). Concentrations of 3 alpha-reduced neuroactive steroids and their precursors in plasma of patients with major depression and after clinical recovery. Biol Psychiatry 45: 274–277.
Suda S, Segi-Nishida E, Newton SS, Duman RS (2008). A postpartum model in rat: behavioral and gene expression changes induced by ovarian steroid deprivation. Biol Psychiatry 64: 311–319.
Tanaka M, Sokabe M (2013). Bidirectional modulatory effect of 17beta-estradiol on NMDA receptors via ERalpha and ERbeta in the dentate gyrus of juvenile male rats. Neuropharmacology 75C: 262–273.
ter Horst GJ (2010). Estrogen in the limbic system. Vitam Horm 82: 319–338.
Uzunova V, Sampson L, Uzunov DP (2006). Relevance of endogenous 3alpha-reduced neurosteroids to depression and antidepressant action. Psychopharmacology 186: 351–361.
Viguera AC, Tondo L, Koukopoulos AE, Reginaldi D, Lepri B, Baldessarini RJ (2011). Episodes of mood disorders in 2,252 pregnancies and postpartum periods. Am J Psychiatry 168: 1179–1185.
Walf AA (2010). Oestrogen receptor beta is involved in the actions of oestrogens in the brain for affective behaviour, but not trophic effects in peripheral tissues. J Neuroendocrinol 22: 141–151.
Walf AA, Frye CA (2005). ERbeta-selective estrogen receptor modulators produce antianxiety behavior when administered systemically to ovariectomized rats. Neuropsychopharmacology 30: 1598–1609.
Walf AA, Koonce CJ, Frye CA (2008). Estradiol or diarylpropionitrile decrease anxiety-like behavior of wildtype, but not estrogen receptor beta knockout, mice. Behav Neurosci 122: 974–981.
Yoo JY, Kim TH, Lee JH, Dunwoodie SL, Ku BJ, Jeong JW (2015). Mig-6 regulates endometrial genes involved in cell cycle and progesterone signaling. Biochem Biophys Res Commun 462: 409–414.
Acknowledgements
We would like to thank The Solomon R and Rebecca D Baker Foundation for their generous support of this research. For the GenRED sample, data and biomaterials were collected in six projects that participated in the NIMH Genetics of Recurrent Early-Onset Depression (GenRED) project. From 1999 to 2003, the principal investigators and co-investigators were New York State Psychiatric Institute, New York, R01-MH060912 (Myrna Weissman, PhD and James K Knowles, MD, PhD); University of Pittsburgh, R01-MH060866 (George S Zubenko, MD, PhD, and Wendy N Zubenko, EdD, RN, CS); Johns Hopkins University, Baltimore, R01-MH059552 (J Raymond DePaulo, MD, Melvin McInnis, MD and Dean MacKinnon, MD); University of Pennsylvania, Philadelphia, R01-MH61686 (Doug Levinson, MD (GenRED coordinator), Madeleine M Gladis, PhD, Kathleen Murphy-Eberenz, PhD and Peter Holmans, PhD (University of Wales College of Medicine)); University of Iowa, Iowa City, R01-MH059542 (Raymond Crowe, MD and William H Coryell, MD); Rush University Medical Center, Chicago, R01-MH059541-05 (William Scheftner, MD, Rush-Presbyterian). Human subjects research was conducted under IRB protocol # 00008149 and 00049309.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
Supplementary information
Rights and permissions
About this article
Cite this article
Osborne, L., Clive, M., Kimmel, M. et al. Replication of Epigenetic Postpartum Depression Biomarkers and Variation with Hormone Levels. Neuropsychopharmacol 41, 1648–1658 (2016). https://doi.org/10.1038/npp.2015.333
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2015.333
This article is cited by
-
Risk Factors for Postpartum Depression Based on Genetic and Epigenetic Interactions
Molecular Neurobiology (2023)
-
DNA methylation-based predictors of health: applications and statistical considerations
Nature Reviews Genetics (2022)
-
Probiotics as a treatment for prenatal maternal anxiety and depression: a double-blind randomized pilot trial
Scientific Reports (2021)
-
Epigenetic signatures of attachment insecurity and childhood adversity provide evidence for role transition in the pathogenesis of perinatal depression
Translational Psychiatry (2020)
-
Precision medicine in perinatal depression in light of the human microbiome
Psychopharmacology (2020)