Abstract
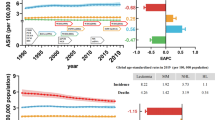
We examined cancer mortality at ages 13–29 years in England and Wales between 1981 and 2005, a total of 20 026 deaths over approximately 303 million person-years (mpy) at risk by sex, age group and time period. Overall, the mortality rate was 65.6 per mpy. Malignant neoplasms of the central nervous system showed the highest rate (8.5), followed by myeloid and monocytic leukaemia (6.6), lymphoid leukaemia (6.4), malignant bone tumours (5.4) and non-Hodgkin's lymphoma (5.2). These groups together accounted for almost 50% of all cancer deaths. The mortality rate for males (72.4) was 23% higher than for females (58.6) (P-value <0.0001). Males showed significantly higher mortality rates than females in almost all diagnostic groups, in general, mortality increasing with age (P-value <0.0001). There were significant decreases in mortality over time, the annual percentage change between 1981 and 2005 being minus 1.86 (95% confidence interval −2.09 to −1.62). Cancer groups with the highest mortality differed from those with the highest incidence.
Similar content being viewed by others
Main
One in four of all deaths in the United Kingdom is caused by cancer (Coleman et al, 1999). Although the majority of these deaths occur in the elderly, cancer represents the most common cause of death at ages 13–29 years. Approximately 2500 teenagers and young adults (TYAs) died from cancer in England and Wales in the 4-year period 2002–2005. Little is known about the aetiology of cancers in such young people, though; it is likely that it differs from that in older adults (Birch, 2005, pp 13–31).
We carried out detailed analyses of mortality rates by cancer group, sex, age and time period in persons aged 13–29 years in England and Wales, to identify the highest mortalities and lowest reductions in mortality over time; these, it is hoped, will assist with targeting of clinical resources and service planning.
Methods
Mortality data on neoplasms in England and Wales from 1981 to 2005 were provided by the Office for National Statistics, London (ONS); those covered malignant neoplasms, benign tumours and neoplasms of uncertain behaviour, in those aged 13–29 years. For each observation, age at death, sex, and diagnosis coded according to the International Classification of Diseases (ICD) were included. Data on cases registered from 1981 to 2001, a period that spans both the ICD Ninth Revision (ICD-9) (World Health Organization, 1977) and ICD Tenth Revision (ICD-10) (World Health Organization, 1992) coding epochs at the ONS, were released by the English Cancer Information System (Office for National Statistics, 2004) along with the tabulation for the conversion from the earlier ICD-9 to ICD-10. Direct translation between ICD-9 and ICD-10 at the 4-digit level for all codes was not possible. We, therefore, used the ICD-10 codes up to the third digit. For comparison purposes, we also considered incidence data on all registered neoplasms diagnosed in England from 1979 to 2003 inclusive, supplied by the National Cancer Intelligence Centre, ONS, London (Office for National Statistics, 2006b).
Mid-year estimates, by single year of age and sex, of the resident population in England and Wales for the time period 1981–2005 were obtained, based on the national censuses (Office for National Statistics, 2007). Number of deaths and population estimates were tabulated by age, sex and time period. The age groups were 13–14, 15–19, 20–24 and 25–29 years. The time span was divided into five quinquennia. Thirteen main diagnostic groups were defined as shown in Table 1, three of which were further subclassified giving 14 groups in all and for each, mortality rates were calculated. The European standard population was used for direct standardisation of the rates (Quinn et al, 2005). Throughout this report rates are given per million person-years (mpy).
Heterogeneity between sexes, age groups, and time periods was tested for by using a χ2 test statistic. Age and temporal trends was tested for, by using a single degree of freedom χ2 statistic (Armitage, 1955); the estimate of the percent change per year of age (PCYA) was obtained by using a linear regression of the natural logarithm of the rates; similarly, in the temporal analysis the annual percent change (APC) was estimated by using a weighted linear regression of the natural logarithm of the age-adjusted rates where the weights were given by the inverse of the estimated variance of the response variable (Kim et al, 2000). Significance level was set at 5%.
The results of the separate stratified analyses were successively assessed with Poisson additive models (Wood, 2006), including main effects, interaction terms, and non-linear temporal trends simultaneously. The statistical analyses were performed using Stata v. 9.2 (StataCorp, 2005) and the software R (R Development Core Team, 2006).
Results
A total of 20 026 deaths were registered over 25-year period in people aged 13–29 years with ICD-10 codes C00-D48, of which 875 were from benign, uncertain or unknown behaviour tumours. There were approximately 303 million person-years at risk. Overall, the mortality rate was 65.6 per mpy (Table 2). Malignant tumours of the central nervous system (CNS) showed the highest mortality rate (8.5), followed by myeloid and monocytic leukaemia (MML) (6.6), lymphoid leukaemia (LL) (6.4), malignant bone tumours (bone) (5.4) and non-Hodgkin's lymphoma (NHL) (5.2). These groups together accounted for almost 50% of all deaths under study.
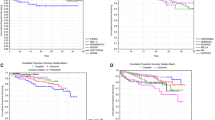
Overall, the mortality rate for males (72.4) was 23% higher than for females (58.6), and significantly higher in all the specified groups except breast and genitourinary (GU) organs, where females had higher rates; there was no significant heterogeneity by sex for liver cancer, melanoma, GU sites other than gonads and cervix, thyroid and non-malignant neoplasms of the CNS. There were large disproportions of rates between males and females for cancers of the lip, oral cavity and pharynx, respiratory organs, bone and lymphomas and leukaemias. In these groups, the ratio of rates in males compared to females was between 1.5 and 2.2.
The mortality differed between age groups for all specified diagnostic groups except thyroid and other endocrine glands (Table 3). The rates for breast and cervical cancer increased by 50% for each additional year of age. Marked increases across age groups were also observed for digestive organs (excluding liver), melanoma of skin and testicular cancer, whereas for bone cancer decreases on average by nearly 8% per year of age, the largest drop among the diagnostic groups. Lymphomas and MML rates increased rates with age, with the largest increases at ages 13–19 years. Mortality for LL peaked at age 15–19 years. For Hodgkin's lymphoma (HL), mortality for persons aged 25–29 years was 11 times higher than the rate for those aged 13–14 years.
When using the Poisson regression approach, few groups showed a significant interaction between sex and age. For bone, the relative risk in males compared to females increased with age, from 0.8 (95% confidence interval, CI, 0.6–1.1) at 13–14 years to 2.1 (95% CI 1.6–2.8) at 25–29 years. For NHL, the relative risk decreased by age, in males being three (95% CI 1.7–5.3) times higher at 13–14 years and 1.7 (95% CI 1.4–2) times higher at 25–29 years.
Mortality for all cancers combined decreased over time by 1.86% on average each year (Table 4). Numbers decreasing from about 1000 per year in 1981–1985 to a little over 600 per year in 2001–2005 period. Testicular cancer showed the largest APC (−6.31), followed by HL (−5.12), cancer of respiratory and intra-thoracic organs (−4.26), and cervical cancer (−4.07). Neither the total nor the sex-specific mortality rates for bone showed a significant trend over time. Further analyses revealed that the rates, after decreasing in the first three time periods, increased in the last 10 years at age 20–24 years (APC 1.43, CI 0.16–2.72); this was also supported by the Poisson regression.
Groups with the highest mortality (CNS, MML, LL, bone, NHL) differed from those with the highest incidence (HL, testis, melanoma, CNS, cervix) (Table 5). CNS, MML, LL, bone and soft tissue were all in the top 10 for mortality and were between 3 and 8 rank places higher than for incidence. The ratio of incidence to mortality varied from 16 : 1 for testis and 11 : 1 for thyroid cancer to where the rates are similar, as for liver. The ratio for MML, LL, and bone was below 2 : 1. Testicular and cervical cancer, melanoma, and HL were among the top five groups with the highest incidence between 1979 and 2003 but below the 5th position for mortality between 1981 and 2005, with deaths numbering much below that of new cases.
In 2002–2005, approximately 2500 TYAs in England died from neoplasms, of which 2341 were coded as malignant, making cancer the commonest disease-related cause of death at these ages, accounting for approximately 12% of all deaths and exceeded only by deaths from transport accidents, though at 13–14 years neoplasmic deaths outnumbered deaths from any other cause (Table 6). Deaths from all causes by sex and age group showed a heterogeneous distribution.
Among the 875 deaths coded as being due to benign (275) or uncertain and unknown behaviour (600) neoplasms, 166 involved endocrine glands, 49 middle ear, respiratory and intrathoracic organs, 57 mesothelial and soft tissue, 31 haemopoietic and 23 of GU organs and 549 other sites.
Discussion
This is the first study to present detailed analyses of cancer mortality in TYAs in England and Wales and makes use of recent national data over a 25-year period. The introduction of ICD-10 in 2001 had an impact on the analysis of trends in cancer mortality (Brock et al, 2004). Comparability ratios provide a measure of the effect of changes in coding practice that may vary by site and age. Approximated estimates of variations in rates of TYA mortality trends showed substantial robustness of the data to the introduction of the ICD-10 coding system. The results demonstrate that cancer mortality in TYAs has decreased over time. Yet, cancer is still the most common disease-related cause of death in this age group. Moreover, the sites of most lethal cancers differ from those at higher ages (Office for National Statistics, 2006a). Some of the deaths due to benign neoplasms or those of uncertain behaviour may have been miscoded or reported inaccurately. However, the small proportion of deaths so assigned to ill-defined sites supports the robustness of the data.
Major mortality reductions occurred for cancers of (i) respiratory and intrathoracic organs, mainly bronchus and lung, (ii) GU organs, cervical and testicular cancer in particular, and (iii) HL; whereas cancers of digestive organs, soft tissue, and CNS showed lower decreases in rates and less favourable incidence to mortality ratios. There were no corresponding incidence falls of these cancers in TYAs and in contrast some temporal increases have been noted (Birch, 2005). The marked reductions in mortality must therefore be due to well-documented improvements in survival, particularly from testis cancer and HL (Coleman et al, 1999). Given our study period, it is likely that cervical screening will have contributed to the reduction in cervix cancer mortality. That from melanoma remained relatively constant over time, in spite of an increase in incidence, and was higher in males. In contrast, incidence was higher in females indicating that survival for melanoma is higher in females and has increased over time. Increased public and physician awareness of melanoma in young people may have contributed to these changes.
Previous national studies of cancer mortality in England and Wales presented data up to 1997 (Swerdlow et al, 2001) and 2003 (Quinn et al, 2001; Rowan et al, 2005) and included figures for broad and variable age groups (e.g. 15–34, 20–44) depending on cancer site. Furthermore, not all relevant cancer sites were reported in detail for example bone, soft tissue, thyroid, HL, MML, LL and liver (Quinn et al, 2001); bone, soft tissue, MML, LL (Swerdlow et al, 2001), thereby preventing direct comparisons. Levi et al (2003) reported mortality trends at 15–24 years in Europe, including the United Kingdom but compared, 1965–1969 with 1995–1998, and only for selected diagnostic groups (bone, soft tissue, testis, NHL, HL, and all leukaemias combined), again, precluding direct comparison.
A recent study from the United States covering the period 1975–2000 included some mortality at ages 15–29 years (Bleyer et al, 2006), but was primarily on incidence and survival. In general, the trends were compatible with the present study though some differences were apparent. Thus, decreases in mortality at 15–29 years were reported for melanoma, colorectal carcinoma and testicular cancers; there were smaller reductions for CNS tumours and breast cancer. For liver cancer there was an overall decrease, but mortality increased in the more recent years, but time trends for other groups were not reported. In the present study, up to year 2000, no reduction in mortality from colorectal cancer was seen, but there was a steady decrease in breast cancer and mortality from liver cancer was stable. These differences may, at least in part, be due to differences in the ethnic mix in the United States, England, and Wales.
The recent guidance on improving outcomes in children and young people with cancer, published by the National Institute for Health and Clinical Excellence (National Collaborating Centre for Cancer, 2005) noted the lack of available comprehensive data on cancers in TYAs. The present report provides this for mortality in England and Wales. The results highlight diagnostic groups, which present the greatest clinical challenges, including those in which the ratio of incidence to mortality is low, indicating poor survival and those groups with little or no reductions in mortality over time. The four leading causes of cancer death, CNS tumours, MML, LL, and bone cancers, all have low incidence to mortality ratios. Furthermore, over the 25-year study period, mortality in CNS and bone tumours has decreased by less than 1%. These observations may assist with resource allocation and the setting of clinical targets.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Armitage P (1955) Tests for linear trends in proportions and frequencies. Biometrics 11: 375–386
Birch JM (2005) Patterns of incidence of cancer in teenagers and young adults: implications for Aetiology. In: Eden TOB, Barr RD, Bleyer A, Whiteston M (eds) Cancer and the Adolescent 2nd edn, London: Blackwell Publishing, pp 13–31
Bleyer A, O'Leary M, Barr R, Ries LAG (eds) (2006) Cancer Epidemiology in Older Adolescents and Young Adults 15–29 Years of Age, Including SEER Incidence and Survival: 1975–2000. Bethesda, MD: National Cancer Institute, NIH
Brock A, Griffiths C, Rooney C (2004) The effect of the introduction of ICD-10 on cancer mortality trends in England and Wales. Office for National Statistics, Health Statistics Quarterly 23: 7–17
Coleman MP, Babb P, Damiecki P, Grosclaude P, Honjo S, Jones J, Knerer G, Pitard A, Quinn M, Sloggett A, De Stavola B (1999) Cancer Survival Trends in England and Wales, 1971–1995: Deprivation and NHS Region Studies in Medical and Population Subjects No 61 London: The Stationery Office
Kim HJ, Fay MP, Feuer EJ, Midthune DN (2000) Permutation test for joinpoint regression with applications to cancer rates. StatMed 19: 335–351, (correction: 2001; 20:655)
Levi F, Lucchini F, Negri E, La Vecchia C (2003) Trends in cancer mortality at age 15–24 years in Europe. Eur J Cancer 39: 2611–2621
National Collaborating Centre for Cancer (2005) Guidance on Cancer Services, Improving Outcomes in Children and Young People with Cancer. London: National Institute for Health and Clinical Excellence
Office for National Statistics (2006a) Mortality Statistics: Cause, England & Wales, 2005 Series DH2 No 32 London: Office for National Statistics
Office for National Statistics (2006b) Cancer Statistics Registrations. Registrations of Cancer Diagnosed in 2004, England Series MB1 No 35 London: Office for National Statistics
Office for National Statistics (2007) Population Estimates for UK, England and Wales, Scotland and Northern Ireland, http://www.statistics.gov.uk/statbase/Product.asp?vlnk=601&More=N accessed 23 February 2007
Office for National Statistics (2004) 1981–2001 ONS ICD9–10 Mortality Data Conversion. Version 1.1, CD-ROM
Quinn M, Babb P, Brock A, Kirby L, Jones J (2001) Cancer Trends in England and Wales 1950–1999 Office for National Statistics London: The Stationery Office
Quinn MJ, Wood H, Cooper N, Rowan S (ed). (2005) Cancer Atlas of the United Kingdom and Ireland 1991–2000. Studies on Medical and Population Subjects No 68 London: Palgrave MacMillan
R Development Core Team (2006) R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing, ISBN 3–900051–07–0 http://www.R-project.org
Rowan S, Wood H, Cooper N, Quinn M (2005) Update to Cancer Trends in England and Wales 1950–1999 Office for National Statistics London: The Stationery Office
StataCorp (2005) Stata Statistical Software: Release 9. College Station, TX: StataCorp LP
Swerdlow A, dos Santos Silva I, Doll R (2001) Cancer Incidence and Mortality in England and Wales. Oxford: Oxford University Press
Wood SN (2006) Generalized Additive Models: An Introduction with R. Boca Raton, FL: Chapman & Hall/CRC
World Health Organization (1977) International Statistical Classification of Diseases Ninth Revision, Volume 1 Geneva: WHO
World Health Organization (1992). International Statistical Classification of Diseases and Related Health Problems, Tenth Revision Volume 1 Geneva: WHO
Acknowledgements
This research was funded by CLIC Sargent. Tim Eden is Teenage Cancer Trust Professor of Teenage and Young Adult Cancer, University of Manchester, Jillian Birch is Cancer Research UK Professorial Fellow, University of Manchester.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Geraci, M., Birch, J., Alston, R. et al. Cancer mortality in 13 to 29-year-olds in England and Wales, 1981–2005. Br J Cancer 97, 1588–1594 (2007). https://doi.org/10.1038/sj.bjc.6604080
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604080
Keywords
This article is cited by
-
UK guidelines for the management of soft tissue sarcomas
Clinical Sarcoma Research (2016)
-
RAF gene fusions are specific to pilocytic astrocytoma in a broad paediatric brain tumour cohort
Acta Neuropathologica (2010)
-
MYB upregulation and genetic aberrations in a subset of pediatric low-grade gliomas
Acta Neuropathologica (2010)
-
Rates of inclusion of teenagers and young adults in England into National Cancer Research Network clinical trials: Report from the National Cancer Research Institute (NCRI) Teenage and Young Adult Clinical Studies Development Group
British Journal of Cancer (2008)
-
Survival from cancer in teenagers and young adults in England, 1979–2003
British Journal of Cancer (2008)