Abstract
Aims: Low molecular weight heparins (LMWHs) are widely used as curative or preventive treatments of thromboembolic diseases. The aim of our study was to: (i) investigate the pattern of prescription of LMWHs in different departments of French teaching hospitals; and (ii) estimate the incidence of adverse drug reactions (ADRs) induced by LMWHs and associated risk factors for the occurrence of bleeding events.
Methods: This prospective study was performed in two teaching hospitals in Toulouse (south-western France) in March 1999 in different medical wards. All patients receiving a prescription for a LMWH were included in the survey. All data were prospectively recorded in each ward.
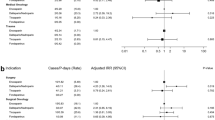
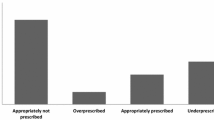
Results: A total of 334 patients were included. Sex ratio (male/female) was 1.25 and mean age was 72.5 ± 16.3 years (extremes: 18–101). 450 prescriptions for LMWHs were collected (1.34 prescription per patient) and involved mainly enoxaparin (61%), which was more frequently used than tinzaparin in patients over 75 years old (71.7 vs 28.3%; p < 0.0001). Ninety-nine patients received a LMWH for curative treatment (corresponding to 127 prescriptions of which 99 were for enoxaparin and 28 were for tinzaparin [p < 0.0001]). Indications included therapy for deep venous thrombosis, pulmonary embolism, acute coronary syndrome, unstable angina pectoris, non-Q-wave myocardial infarction. Serious renal insufficiency was significantly more frequent in patients from the geriatrics department (p < 0.00001). Enoxaparin was prescribed more frequently in patients with serious or moderate renal insufficiency than tinzaparin (72 vs 61%, p < 0.05). The incidence of LMWHs-induced ADRs was 10.5% occurring in 22 cases during preventive treatment of deep venous thrombosis and in 13 cases during curative therapy. ADRs were classified as ‘serious’ in 11 cases (31.4%). Reported ADRs were bleeding events (n = 15), thrombocytosis (n = 13), thrombopenia (n = 4) and hepatic cytolysis (n = 1). The mean delay for the occurrence of bleeding effects was 8.0 ± 9.1 days (range 1–40). Multivariate analysis of the influence of several criteria on the occurrence of haemorrhagic effects showed that the decrease of creatinine clearance (10 ml/min) was associated with an increased haemorrhagic risk (relative risk [RR] = 1.34, 95% CI 1.12–1.65; p < 0.05). Moreover, the risk of adverse bleeding effects increased for patients with a creatinine clearance <20 ml/min (RR = 2.8; 95% CI 1.00–7.8).
Conclusion: Our data firstly show a different pattern of LMWHs prescription in different clinical wards. Secondly, the risk of bleeding ADRs in patients treated by LMWHs increases significantly with renal function impairment for the two LMWH preparations studied. More pharmacoepidemiological studies are necessary in patients with several risk factors, particularly in elderly people who often have renal impairment, in order to determine the optimal pattern use of each LMWH.





Similar content being viewed by others
References
Clagett GP, Anderson FA, Geerts W, et al. Prevention of VTE. Chest 1998; 5: 531S–60S
Sandler DA, Martin JF. Autopsy proven pulmonary embolism in hospital patients: are we detecting enough deep vein thrombosis? J R Soc Med 1989; 82: 198–200
Leizorovicz A, Haugh MC, Chapuis FR, et al. Low molecular weight heparin in prevention of perioperative thrombosis. BMJ 1992; 305: 913–20
Nurmohamed MT, Rosendaal FR, Büller HR, et al. Low molecular weight heparin versus standard heparin in general and orthopaedic surgery: a metanalysis. Lancet 1992; 340: 152–6
Leizorovicz A, Simmoneau G, Decousus H, et al. Comparison of the efficacy of low molecular weight heparins and unfractionated heparin in the initial treatment of deep venous thrombosis: a meta-analysis. BMJ 1994; 309: 299–304
Lensing AWA, Prins MH, Davidson BL, et al. Treatment of deep venous thrombosis with low molecular weight heparins: a meta-analysis. Arch Intern Med 1995; 6: 601–7
Dolovich LR, Ginsberg JS, Douketis D, et al. A meta-analysis comparing low-molecular-weight-heparins with unfractionated heparin in the treatment of venous thromboembolism. Arch Intern Med 2000; 2: 181–8
Simonneau G, Sors H, Charbonnier B, et al. A comparison of low molecular weight heparin with unfractionated heparin for acute pulmonary embolism. N Engl J Med 1997; 337: 663–9
Klein W, Buchwald A, Hillis SE, et al. Comparison of low molecular weight heparin with unfractionated heparin acutely and with placebo for 6 weeks in the management of unstable coronary artery disease. Fragmin in Unstable Coronary Disease study (FRISC). Circulation 1997; 96: 61–8
Cohen M, Demers C, Gurfinkel EP, et al. A comparison of low molecular weight heparin with unfractionated heparin for unstable coronary artery disease. N Engl J Med 1997; 337: 447–52
Samama MM, Cohen. T, Darmon J, et al. A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely III medical patients. N Engl J Med 1999; 341: 793–800
Maguire P, Selby P. Assessing quality of life in cancer patients. Br J Cancer 1989; 60: 437–40
Dictionnaire Vidal. Editions du Vidal — OVP. Paris, 1999
Begaud B, Evreux JC, Jouglard J, et al. Imputabilité des effets inattendus ou toxiques des médicaments [in French]. Thérapie 1985; 40(2): 111–8
Edwards IK, Aronson JK. Adverse drug reactions: definitions, diagnosis and management. Lancet 2000; 356: 1225–9
Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron 1976; 16: 31–41
Guide National de Prescription. Editions du Vidal — OVP. Paris, 2000
Levine MN, Raskob G, Landefeld S, et al. Hemorrhagic complications of anticoagulant treatment. Chest 1998; 114: 511S–23S
White RH, Beyth RJ, Zhou H, et al. Major bleeding after hospitalization for deep-venous thrombosis. Am J Med 1999; 107: 414–24
Palareti G, Leali N, Coccheri S, et al. Bleeding complications of oral anticoagulant treatment: an inception cohort, prospective collaborative study. Lancet 1996; 348: 423–8
Callaert S, Chouaid C, Causse R, et al. Evaluation de la prescription des héparines de bas poids moléculaire au centre hospitalier intercommunal de Créteil. Thérapie 1998; 53: 587–90
Thilly N, Pierson H, Collard C, et al. Prévention de la maladie thromboembolique veineuse en milieu médical: de l’aide à la décision à l’utilisation des héparines de bas poids moléculaire. Thérapie 1998; 53: 579–86
Thromboembolic Risk Factors (THRIFT) Consensus Group. Risk of and prophylaxis for venous thromboembolism in hospital patients. BMJ 1992; 6853: 567–74
Campbell NRC, Hull RD, Brant RF, et al. Aging and heparin-related bleeding. Arch Intern Med 1996; 156: 857–60
Nieuwenhuis HK, Albada J, Banga JD, et al. Identification of risk factors for bleeding during treatment of acute venous thromboembolism with heparin or low molecular weight heparin. Blood 1991; 78: 2337–43
Landefeld CS, Cook EF, Flatley M, et al. Identification and preliminary validation of predictors of major bleeding in hospitalized patients starting anticoagulant therapy. Am J Med 1987; 82: 703–13
Bonnet F, Morlat P, de Witte S, et al. Accidents hémorragiques des héparines de bas moléculaire: 15 observations. Rev Med Interne 2001; 22: 761–3
Grateau G, Chauvenet L, Oudard S, et al. Accidents hémorragiques graves lors d’un traitement par héparine de bas poids moléculaire: a propos de 2 observations. Rev Med Interne 1997; 18: 411–5
Manckoundia P, Zarouala B, lalu-Fraisse A, et al. Hématomes musculaires chez le sujet très âgé lors d’un traitement par héparine de bas poids moléculaire [letter]. Presse Med 2000; 29: 702
Goudable C, Saivin S, Houin G, et al. Pharmacokinetics of a low molecular weight heparin (Fraxiparine) in various stages of chronic renal failure. Nephron 1991; 59: 543–5
Mismetti P, Laporte-Simitsidis S, Navarro C, et al. Aging and venous thromboembolism influence the pharmacodynamics of the anti-factor Xa and anti-thrombin activities of a low molecular weight heparin (nadroparin). Thromb Haemost 1998; 79: 1162–5
Gerlach AT, Pickworth KK, Seth SK, et al. Enoxaparin and bleeding complications: a review in patients with and without renal insufficiency. Pharmacotherapy 2000; 7: 771–5
Cadroy Y, Pourrat J, Baladre MF, et al. Delayed elimination of enoxaparine in patients with chronic renal insufficiency. Thromb Res 1991; 63: 385–90
Collet JP, Montalescot G, Choussat R, et al. Enoxaparin in unstable angina patients with renal failure [abstract]. Arch Mal Coeur Vaiss 2002; 95: 119
Siguret V, Pautas E, Fevrier M, et al. Elderly patients treated with tinzaparin (Innohep) administered once daily (175 antiXa IU/kg): anti-Xa and anti-Iia activities over 10 days. Thromb Haemost 2000; 84: 800–4
Harenberg J, Huhle G, Piazolo L, et al. Long term anticoagulation of outpatients with adverse events to oral anticoagulants using low molecular weight heparin. Semin Thromb Hemost 1997; 23(2): 167–72
Monreal M, Roncales FJ, Ruiz J, et al. Secondary prevention of venous thromboembolism: a role for low molecular weight heparin. Haemostasis 1998; 28: 236–43
Layton D, Clark DW, Pearce GL, et al. Is there an association between selective serotonin reuptake inhibitors and risk of abnormal bleeding? Results from a cohort study based on prescription event monitoring in England. Eur J Clin Pharmacol 2001; 2: 167–76
Bottlender R, Dobmeier P, Moller HJ. The effect of selective serotonin-reuptake inhibitors in blood coagulation. Fortschr Neurol Psychiatr 1998; 1: 32–5
Rizzieri DA, Wong WM, Gockerman JP. Thrombocytosis associated with low molecular weight heparin [letter]. Ann Intern Med 1996; 2: 157
Williams E. Thrombocytosis associated with low molecular weight heparin. Ann Intern Med 1997; 9: 742–3
Ziaja K, Simka M, Krupowies A, et al. Thrombocytosis after prophylactic administration of enoxaparin: unexpected findings in a Polish prospective multicenter trial on the efficacy and safety of enoxaparin in the prevention of postoperative thromboembolism. Int Angiol 1999; 1: 65–9
Liautard Ch, Correa Nunes AM, Vial T, et al. Low-molecular-weight heparins and thrombocytosis. Ann Pharmacother 2002; 36: 1351–4
Shen ZX, Basara N, Xi XD, et al. Fraxiparin, a low-molecular-weight heparin, stimulates megakaryocytopoiesis in vitro and in vivo mice. Br J Haematol 1994; 88: 608–12
Bollinger KA, Vermeulen LC, Davis S, et al. Comparative effectiveness of low-molecular-weight heparins after therapeutic interchange. Am J Health Syst Pharm 2000; 57: 368–72
Turpie AGG. Can we differentiate the low molecular weight heparins? Clin Cardiol 2000; 23: 14–7
Bara L, Planes A, Samama MM. Occurrence of thrombosis and haemorrage, relationship with anti-Xa, anti-Iia activities, and D-dimer plasma levels in patients receiving a low molecular weight heparin, enoxaparin or tinzaparin, to prevent deep vein thrombosis after hip surgery. Br J Haematol 1999; 104: 230–40
Low Molecular Weight Heparins and Haemorrhagic Risk. French Drug Agency [letter]. Available from URL: http://www.agmed.sante.gouv.fr. [Accessed 2000 Sep 1]
French Drug Agency. [press conference]. Available from URL: http://www.agmed.sante.gouv.fr. [Accessed 2002 Apr 10]
Acknowledgements
The authors have provided no information on sources of funding or on conflicts of interest directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cestac, P., Bagheri, H., Lapeyre-Mestre, M. et al. Utilisation and Safety of Low Molecular Weight Heparins. Drug-Safety 26, 197–207 (2003). https://doi.org/10.2165/00002018-200326030-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200326030-00005