ABSTRACT
An estimated 10% of COVID-19 survivors continue to experience symptoms several weeks to months after the appearance of initial symptoms, a condition termed post-acute sequelae of SARS-CoV-2 infection (PASC). These patients, also called “long-haulers,” most commonly report protracted symptoms of fatigue, cough, dyspnea, chest tightness, difficulty concentrating, arthralgia, olfactory dysfunction, and headache. While age, comorbid medical conditions, and COVID-19 severity are suspected risk factors for PASC, young and previously healthy individuals with mild COVID-19 are also at risk. Recognition of symptoms, evaluation, supportive treatment, and attention to medical comorbidities are the cornerstones of medical management.
If COVID-19 symptoms persist for more than 4 weeks, patients should be assessed for pulmonary, cardiac, neurocognitive, and psychiatric complications.
In patients with post-acute sequelae of SARS-CoV-2 infection, symptoms may persist for more than 6 months.
Focus treatment on managing symptoms, comorbidities, pulmonary rehabilitation, and continued follow-up.
INTRODUCTION
As the COVID-19 pandemic continues globally, there is increasing need to understand the entire disease spectrum and anticipate long-term management of survivors. Early in the pandemic, adults with mild to moderate COVID-19 were believed to have a short-term course of acute illness lasting approximately 2 weeks, after which symptoms completely resolved. However, emerging data have described a subgroup of patients with a prolonged course of symptoms lasting several weeks to months.1
This protracted form of COVID-19 has been given several descriptive names, including post-acute COVID-19 syndrome, long COVID, and long-haul COVID-19, with affected patients termed “long-haulers.” However, the National Institutes of Health (NIH) recently called for a consensus term to describe this protracted form of COVID-19, now termed post-acute sequelae of SARS-CoV-2 infection (PASC).2 Although the definition seems to be evolving and is not yet formalized, PASC is currently recognized if symptoms persist for at least 28 days after onset of COVID-19 symptoms. By building a consensus definition and terminology for PASC, the NIH aims to increase grant funding to research initiatives to investigate PASC and, hopefully, determine treatment.2
PASC should be recognized among other sequelae affecting COVID-19 survivors. For example, the post-intensive care syndrome (PICS) describes a distinct group of patients who develop new or worsening cognitive, physical, or psychiatric health impairments after suffering critical COVID-19 symptoms requiring admission to the intensive care unit (ICU).3 In contrast, PASC can apply to the broad range of COVID-19 survivors, from those with mild acute illness who may have never required hospitalization to ICU survivors. Survivors of critical illness associated with COVID-19 can be viewed as likely having an overlap of PICS and PASC as part of the spectrum of post-COVID-19 complications.
TRUE NUMBERS ARE HARD TO ASSESS
A marked variability in reported symptoms, duration, and definitions of COVID-19 sequelae in studies makes it difficult to estimate the true incidence of PASC. However, by some estimates, at least 10% of patients who test positive for COVID-19 experience symptoms for longer than 3 weeks.4
Although advanced age, obesity, comorbid psychiatric conditions, and other chronic medical conditions are suspected risk factors for PASC, nearly 20% of cases are in adults ages 18 to 34 with no chronic medical conditions.5 The incidence of PASC may be higher in populations of racial and ethnic minorities and in groups predisposed to disparities in social determinants of health.6 Studies that included hospitalized patients report the highest prevalence of protracted symptoms, with data suggesting more than two-thirds of these patients have continued symptoms 6 months after recovery from acute COVID-19.7,8 Data are insufficient to directly attribute PASC to prolonged symptoms rather than to other causes of protracted symptoms in hospitalized patients, such as PICS. The prolonged symptoms are likely multifactorial and may be difficult to attribute to a single cause.
MECHANISMS PROPOSED, BUT PATHOPHYSIOLOGY UNKNOWN
The pathophysiology of PASC is not known. Clinicians and researchers are exploring possibilities of a persistent hyperinflammatory state, inadequate antibody response, ongoing viral activity, and organ damage as a reflection of acute insult from the infectious phase.9 Complications of a hypercoagulable state, immunologic aberrations, inflammatory changes, and maladaptation of the angiotensin-converting enzyme 2 pathway may also contribute.10
Mitochondrial dysfunction and metabolic changes are also under investigation because of proposed similarities to myalgic encephalomyelitis and chronic fatigue syndrome.11 Dysautonomia as a neurological complication of PASC has also been hypothesized as a contributing factor to fatigue and hypoxia.12
Some hypothesize that higher viral load exposures increase the risk of PASC.13 Furthermore, it is likely that this syndrome represents a multifactorial presentation attributable to symptoms of underlying medical conditions, features of the acute disease state, and symptoms associated with physical deconditioning from precautionary isolation measures and acute illness.9
Despite the lingering symptoms, the US Centers for Disease Control and Prevention (CDC) reports that most immunocompetent patients with mild to moderate COVID-19 are unlikely to be contagious at 10 days after symptom onset or at 20 days for most immunocompromised patients and patients with severe illness, which allows for discontinuation of isolation precautions at those time points.14,15
A RANGE OF SYMPTOMS
Patients with PASC commonly range in disease severity from outpatients with mild to moderate disease severity to hospitalized patients with severe COVID-19 with or without ICU admission.1,9 Most studies to date have recognized symptoms consistent with PASC persisting after at least 14 to 21 days. Emerging reports are recognizing PASC as persisting symptoms at 28 days in COVID-19 survivors, although an official definition has not been clearly delineated.
The most commonly reported symptoms are fatigue, cough, shortness of breath, chest pain, difficulty concentrating, arthralgia, low-grade fever, and headache (Table 1).7–9,16 Other reported symptoms include cognitive impairment (“brain fog”), olfactory and gustatory dysfunction, sleep difficulty, depression, anxiety, gastrointestinal upset, rashes, alopecia, and palpitations.4,7 In a multinational study of 1030 patients with 331 cases of dermatologic manifestations, pernio (“COVID toes”) was observed in 103 patients, persisting at 60 days after diagnosis in 7% of them.17
Prevalence of COVID-19 symptoms in a series of 143 cases
Two studies noted symptoms at the 60-day follow-up in more than two-thirds of patients recovering from COVID-19.7,8 In a study from Italy, Carfi et al7 found that at 60 days after onset of COVID-19 symptoms, only 18 (12.6%) of 143 patients were completely free of any COVID-19–related symptom, 32% had 1 or 2 symptoms, and 55% had 3 or more symptoms. In a study from Michigan, PASC prevalence was 40% higher in hospitalized versus non-hospitalized patients and twice as likely in patients with severe symptoms at 30 days.13 However, persistent symptoms were still quite prevalent at 60 days in 26.9% of non-hospitalized patients and in 24.5% of in-patients who reported mild illness of the 593 analyzed survey responses.13
In another study of outpatients with COVID-19,5 35% had not returned to their baseline health 2 to 3 weeks following positive testing for SARS-CoV-2.5 Even in previously healthy patients, approximately 20% of patients ages 18 to 34 without chronic medical conditions who were diagnosed with mild COVID-19 not requiring hospitalization reported that they hanot returned to their baseline state of health 2 to 3 weeks after testing.5 Further, patients with dermatologic-dominant and otherwise mild COVID-19 have been reported to manifest dermatologic signs of pernio or livedo reticularis for as long as 150 days from initial diagnosis, again demonstrating the range of initial disease severity that variably becomes PASC.17
Other studies have shown at least 1 persistent symptom, most commonly fatigue or dyspnea, in more than half of patients at 110 days or 180 days, suggesting the longest duration has yet to be determined.18,19,20 Huang et al,20 reporting on patients 6 months after their acute COVID-19 diagnosis, noted continued fatigue in 63%, sleep difficulties in 24%, and anxiety or depression in 23%. The level of persistent lung diffusion impairment and exercise intolerance at 6 months correlated with the severity of COVID-19 illness.
PASC has also had significant global economic impact. A single-center study in France reported that more than 25% of previously active workers (n = 41) discharged from the hospital ward (without ICU stay) had not returned to work after 110 days (mean 110.9 days).18 An observational cohort study of patients discharged after recovery from COVID-19 in Michigan showed that 40% of previously employed individuals had not returned to work and that another 15% returned with reduced hours or responsibilities at 60-day follow-up.20
EVALUATION OF LONG-HAULERS
Guidelines for evaluation of PASC are being developed. Several large centers have created post-COVID-19 clinics that offer a multidisciplinary approach to evaluation and management, including follow-up for noncritically ill patients and post-ICU care. Most clinics accept COVID-19 patients referred for persistent symptoms 1 month after symptom onset. Most use multiple screening measures, including the Montreal Cognitive Assessment, Hospital Anxiety and Depression Scale, and Impact of Event Scale-6, in addition to medication reconciliation, screening for rehabilitation needs, and pulmonary function testing.21 A Post-COVID-19 Functional Status Scale has been created to grade the severity of symptoms, but it has not been validated or widely implemented.22
Interim guidance of the CDC promotes comprehensive assessment and the importance of setting achievable goals with shared decision-making.6 Multidisciplinary care teams typically include primary care, pulmonology, cardiology, infectious disease, neuropsychiatry, behavioral health, social work, physical and occupational therapy, pharmacy, and case management, but their involvement varies depending on particular needs of the patient. Sequelae of COVID-19 are also reportedly affecting the hematologic, renal, endocrine, gastrointestinal and hepatobiliary, rheumatologic, immunologic, and dermatologic organ systems emphasizing the need for coordination of care and support for these patients and their care teams.10
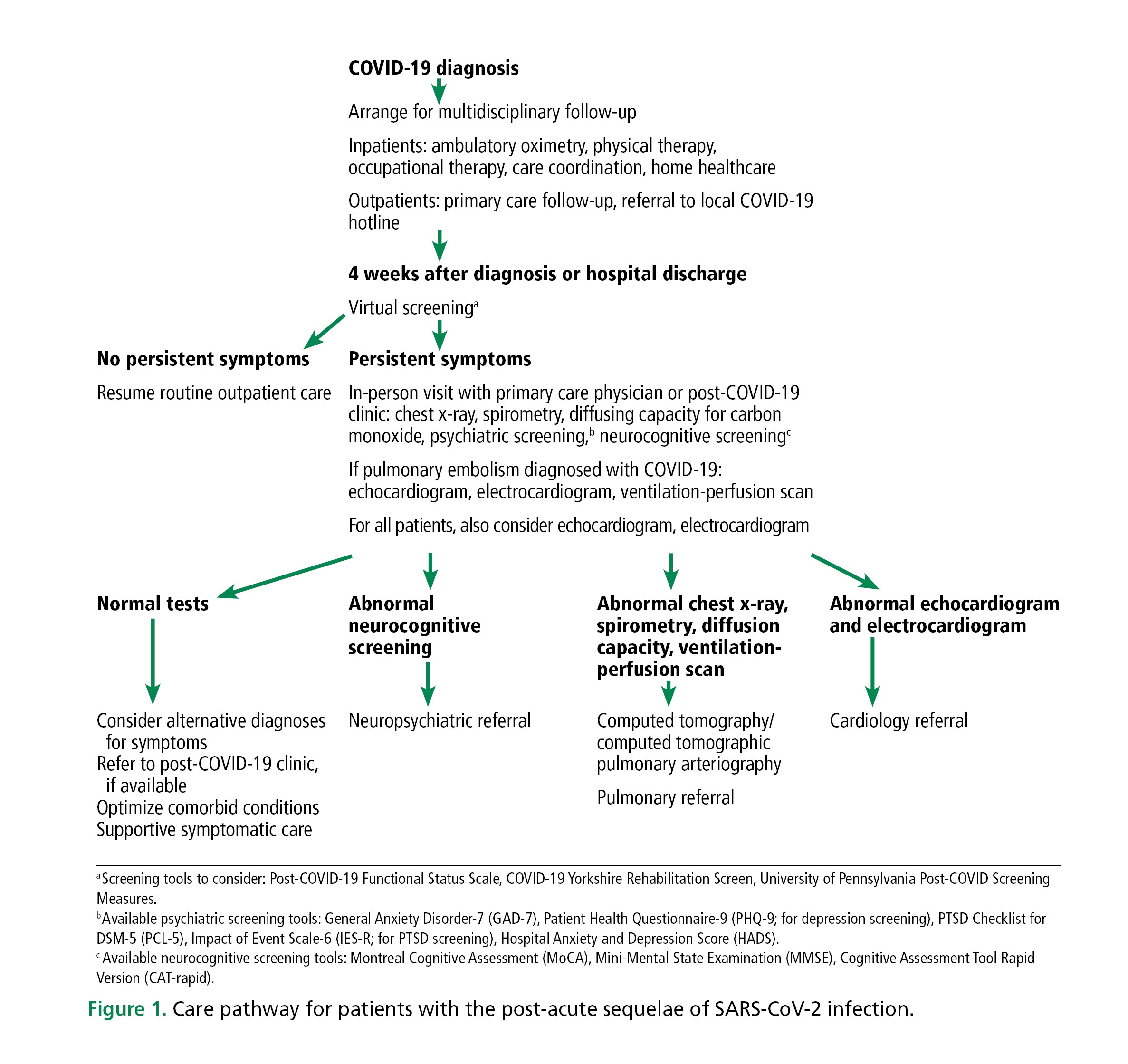
The British Thoracic Society published a guidance algorithm23 suggesting a follow-up chest radiograph at 12-week follow-up. However, timing of imaging tests must be tailored to the individual patient, with some algorithms suggesting chest radiography or computed tomography at 1 month. Our approach to follow-up evaluation and care is shown in Figure 1.
Care pathway for patients with the post-acute sequelae of SARS-CoV-2 infection.
Evaluation of persistent or changing symptoms in patients recovering from COVID-19 should be done comprehensively but also judiciously. COVID-19 may unmask or exacerbate underlying disease processes such as chronic lung disease or cardiovascular disease and may serve as motivation to seek medical care for patients who may not typically schedule routine visits. Basic management of chronic medical conditions is important.
SPECIFIC TREATMENT FOR SYMPTOMS AND COMORBID CONDITIONS
At present, there are no specific treatments for PASC, recognition of this syndrome is a key step toward seeking targeted treatment.
Management focuses on specific treatment of the most bothersome symptoms, such as fatigue or cognitive impairment. Many clinicians are relying on guidelines and strategies used to treat related conditions, although efficacy data and consensus are lacking for cases related to COVID-19. Thus, caution, frequent reassessments, and further studies are needed. For example, patients who develop a presentation typical of organizing pneumonia following COVID-19 infection are commonly managed in accordance with guidelines for organizing pneumonia, utilizing high-dose or prolonged courses of steroids. Cognitive behavioral therapy and graded exercise therapy have been suggested given the benefit in possibly related entities of myalgic encephalomyelitis/chronic fatigue syndrome; however, others caution implementing graded exercise therapy for PASC patients owing to concern of worsening post-exertional malaise.24
Given the complexity and lingering associated symptoms and their impact on several major organ systems, frequent routine follow-up, establishing rapport, and involving a patient’s support system serve as the foundation of management in these patients. A comprehensive, multidisciplinary approach that incorporates detailed management of comorbid medical conditions is the cornerstone of care. Referral to a dedicated post-COVID-19 clinic is recommended, if available.
VACCINATION
Vaccination against SARS-CoV-2 is highly recommended. An initial international survey has shown that more than 50% of PASC patients reported improvement in symptoms following vaccination while a much smaller percentage of less than 10% reported feeling worse.25 Data is also emerging that fully vaccinated patients who develop a “breakthrough” COVID-19 infection are substantially less likely to develop PASC compared with an unvaccinated individual.26 Taken together, these data support vaccination efforts not only to primarily prevent COVID-19 and PASC but also to improve symptoms in patients who already have PASC.
LIMITATIONS OF CURRENT DATA, AND LESSONS LEARNED
There are significant limitations in research efforts to understand the natural history of a pandemic that is almost 2 years old. Limitations include the relatively short time frame of follow-up and a heavy reliance on survey-reporting owing to infection-prevention measures that limit in-person follow-up visits.
Reflecting on lessons learned from the outbreaks of severe acute respiratory distress syndrome and Middle East respiratory syndrome, both caused by related coronaviruses, clinicians should anticipate at least a similar range of long-term effects. Survivors of severe acute respiratory distress syndrome and Middle East respiratory syndrome have been found to have persistent respiratory compromise with abnormal pulmonary function test results, abnormal chest imaging, increased prevalence of psychological conditions, and fatigue that lasted several months.27 Mainstays of their treatment included management of comorbid conditions, pulmonary rehabilitation, and ongoing multidisciplinary follow-up aimed at recognizing impairments and improving outcomes.
FUTURE DIRECTIONS
As part of the PASC initiative, the NIH committed more than $1 billion in grant funding toward several research initiatives to streamline efforts of the medical and scientific communities to improve understanding and treatment of PASC. The SARS-CoV-2 Recovery Cohort will be established as a core resource to help investigate PASC as an important public health concern.
Several studies are proposed or under way to investigate specific treatment including antihistamines, antidepressants, steroids, non-steroidal anti-inflammatory drugs, antioxidants, stimulants, montelukast, melatonin, prolonged thromboprophylaxis, and hyperbaric oxygen.24 Dietary supplementation and probiotics including a trial high-dose vitamin C and two trials examining nicotinamide riboside are ongoing.24 Studies of inflammatory modulators such as the CC ligand-5 blocker leronlimab and anti-interleukin-6 tocilizumab are also under way.24 Exercise regimens and cognitive behavioral therapy are also being investigated. Efforts to increase vaccination and primary prevention remain important.
Establishing ongoing research as well as support for multidisciplinary care teams involved is imperative.
DISCLOSURES
The authors report no relevant financial relationships which, in the context of their contributions, could be perceived as a potential conflict of interest.
Footnotes
The statements and opinions expressed in COVID-19 Curbside Consults are based on experience and the available literature as of the date posted. While we try to regularly update this content, any offered recommendations cannot be substituted for the clinical judgment of clinicians caring for individual patients.
- Copyright © 2021 The Cleveland Clinic Foundation. All Rights Reserved.